When it comes to starting a family, there are many decisions you must make. One of those decisions is choosing a sperm donor. While this may seem like a straightforward process, it is crucial to prioritize the protection of one's health. There has been increased discussion and visibility of natural insemination (NI) in recent years, mainly due to online platforms and forums that connect individuals seeking sperm donors. While some people may choose natural insemination for various reasons, you should consider this method's potential risks. Opting for a sperm bank and artificial insemination (AI) can increase safety and peace of mind.
Key Takeaways
- Natural insemination carries risks of sexually transmitted infections and unwanted pregnancies.
- Choosing a sperm bank provides quality control measures and screening/testing of donors.
- Donor anonymity and confidentiality are maintained, but recipients can access medical history and donor profiles.
- Legal protections exist for both donors and recipients in the sperm bank process.
- Artificial insemination can provide better chances of pregnancy.
- While cost and accessibility may vary, making an informed decision for your health is crucial.
What is Natural Insemination?
Natural insemination refers to the process of conceiving a child through sexual intercourse with a sperm donor. Unlike sperm banks, natural insemination involves direct contact between the donor and the recipient. While some individuals may prefer this method due to its perceived intimacy, it is essential to consider the potential risks involved.
The Risks of Natural Insemination
When it comes to natural insemination, there are several health risks that both donors and recipients should be aware of. Firstly, there is an increased risk of sexually transmitted infections (STIs) as there is direct contact between the donor and recipient. Additionally, there is a lack of quality control and screening measures in place, which can lead to potential genetic disorders or other health complications for the child.
From a legal standpoint, natural insemination poses risks for both parties. Donors may face unexpected legal responsibilities and obligations towards the child without proper legal agreements. Similarly, recipients may encounter difficulties establishing legal parentage or obtaining financial support from the donor.

The Benefits of Choosing AI Over NI
| Benefit | Assisted Hatching May Benefit: |
| Increased chances of conception | Sperm banks offer a wide selection of healthy and viable sperm, increasing the chances of successful conception. |
| Screened donors | Sperm banks thoroughly screen and test their donors for genetic and infectious diseases, ensuring the safety of the recipient and any resulting offspring. |
| Privacy and anonymity | Sperm banks offer the option to donate anonymously, allowing recipients to maintain their privacy and avoid potential legal or emotional complications. |
| Access to medical history | Sperm banks provide detailed medical histories and updated reports of their donors, allowing recipients to make informed decisions about their choice of donor and potential health risks. |
| Convenient and flexible scheduling | Sperm banks offer flexible scheduling options for donors and recipients, making sperm donation and insemination more convenient and accessible. |
Opting for a sperm bank offers numerous benefits when compared to natural insemination. Firstly, sperm banks provide increased safety and protection for donors and recipients. Sperm samples are thoroughly screened and tested for genetic disorders, infectious diseases, and other health conditions before being made available for use. This rigorous screening process significantly reduces the risk of passing on hereditary diseases or infections to the child.
Furthermore, sperm banks offer access to high-quality sperm from carefully selected donors. Donors undergo extensive screening, including medical and psychological evaluations, to ensure suitability. These screenings ensure that recipients have access to sperm from healthy individuals with desirable genetic traits, increasing the chances of a successful pregnancy.
Quality Control Measures in Sperm Banks That You Won't Get Through Natural Insemination
Sperm banks prioritize quality control measures to ensure the health and safety of recipients. The screening and testing process for sperm donors is comprehensive and stringent. Donors are required to undergo thorough medical examinations, including genetic testing, to identify any potential health risks. Additionally, they receive screenings for infectious diseases such as HIV, hepatitis, and syphilis.
Sperm samples are also subject to strict quality control measures. They are tested for motility, viability, and concentration to ensure their suitability for fertility treatments. By implementing these quality control measures, sperm banks assure recipients that they receive sperm from healthy and viable donors.
Screening and Testing of Donors
The screening and testing process for sperm donors ensures the health and well-being of recipients and their future children. Donors must undergo a series of evaluations to assess their physical and mental health. These evaluations include a comprehensive medical history review, physical examinations, and genetic testing.
Genetic testing is vital in identifying potential hereditary diseases that could affect future children. Donors receive screenings for conditions including cystic fibrosis, sickle cell anemia, and various genetic disorders. By conducting these tests, sperm banks can provide recipients with valuable information about the genetic health of their chosen donor.
Donor Anonymity and Confidentiality
Donor anonymity and confidentiality are essential considerations when choosing a sperm donor. Sperm banks prioritize the protection of donor identities to ensure their privacy. This anonymity allows donors to contribute without fear of future legal or emotional obligations towards the child.
Recipients also benefit from donor anonymity, as it allows them to make decisions about their family without external interference. It will enable them to focus on their desires and preferences when selecting a donor without feeling obligated to establish a relationship with the donor in the future.
Access to Donor Information and Medical History
One of the significant advantages of using a sperm bank is the access recipients have to comprehensive donor information and medical history. Sperm banks maintain detailed profiles for each donor, including physical characteristics, educational background, and personal interests. This information allows recipients to choose a donor who aligns with their preferences and values.
Furthermore, recipients have access to the donor's medical history. This information includes any known or newly developed genetic conditions or family health issues. This information is invaluable in understanding potential health risks for the child and making informed decisions about their future well-being.
Diversity of Donor Profiles
Sperm banks offer an extensive range of donor profiles, ensuring recipients have a diverse selection. Donors come from various ethnic backgrounds, allowing recipients to find a donor who shares their cultural heritage. Diversity is crucial for those who want to preserve their cultural roots or guarantee their offspring will inherit a varied genetic makeup.
The availability of diverse donor profiles also ensures that recipients can find donors who possess specific physical traits or talents they desire for their child. Whether it is eye color, height, or musical abilities, sperm banks provide an extensive selection to cater to individual preferences.
Legal Protections for Donors and Recipients
When using a sperm bank, both donors and recipients are protected by legal frameworks. This framework shields donors from legal responsibilities or obligations towards the child conceived through their donation. Recipients, on the other hand, are provided with legal protections regarding parentage and financial support.
These legal protections provide peace of mind for both parties involved, ensuring they can make decisions about their family without fear of future legal complications or disputes.
Cost and Accessibility of Sperm Banks
While the cost of using a sperm bank may be higher compared to natural insemination, the long-term benefits and peace of mind it provides make it worth the added costs. Sperm banks offer various pricing options, allowing recipients to choose a plan that suits their budget. Additionally, many sperm banks provide financing options to make the process more accessible.
Regarding accessibility, sperm banks have a vast network of locations, making it easier for individuals to access their services. These expansions ensure that individuals from different geographical areas have equal opportunities to choose a suitable donor and start their journey toward parenthood.
Choosing A Sperm Bank Over Natural Insemination For Your Health
Protecting one's health should be a top priority when choosing a sperm donor. While natural insemination may seem appealing due to its perceived intimacy and low costs, it comes with significant risks, both in terms of health and legality. Opting for a sperm bank provides increased safety and protection for both donors and recipients.
Sperm banks implement rigorous quality control measures, including comprehensive screening and testing processes for donors. Testing ensures recipients access high-quality sperm from healthy individuals with desirable genetic traits. Additionally, sperm banks offer valuable donor information and updated medical history, allowing recipients to make informed decisions about their future families.
By choosing a sperm bank over natural insemination, you can ensure optimal health and safety while embarking on parenthood. Making a calculated decision that considers long-term implications and provides the best possible outcome for all parties involved is crucial.
Natural Insemination and Artificial Insemination FAQ
What is a sperm bank?
A sperm bank is a facility that collects, freezes, and stores sperm from donors for use in artificial insemination procedures, such as IUI, ICI, IVF, ICSI, and home insemination.
What are the benefits of choosing a sperm bank over natural insemination?
Choosing a sperm bank over natural insemination can provide several benefits. These benefits include access to a wide range of donors, increased control over the selection process, and reduced risk of sexually transmitted infections and passing on genetic conditions.
Does natural insemination have a higher success rate than artificial insemination?
No scientific evidence suggests that natural insemination's success rate is higher than artificial insemination. Artificial insemination techniques have been developed and refined over many years to maximize the chances of successful conception. They allow for controlled and precise placement of sperm, which can increase the likelihood of fertilization.
Is using a sperm bank more expensive than natural insemination?
The cost of natural insemination can vary depending on the donor and the specific arrangement. Some NI donors may offer their services for free, while others may charge a fee. Using a sperm bank can be expensive, with costs ranging from $500 to $10,000 per cycle. However, many insurance plans cover the costs of fertility treatments, and many sperm banks offer financing options.
Can I choose the physical characteristics of the sperm donor?
Many sperm banks provide childhood and adult photos of each donor, allowing recipients to select donors based on physical characteristics. They also offer photo-matching services so recipients can choose a donor that closely resembles their physical traits.
Is using a sperm bank safe?
Using a reputable sperm bank is safe. They are regulated and inspected by the Food and Drug Administration (FDA) and Clinical Laboratory Improvement Amendments (CLIA) to ensure optimal safety. Additionally, sperm is stored and handled in a controlled environment to prevent the risk of contamination or infection.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is CMV?
CMV, cytomegalovirus, is a member of the herpesvirus family and is highly prevalent worldwide. You can become infected with CMV through bodily fluids, including saliva, urine, blood, seminal fluid, and breast milk. The most common transmission modes are through close contact with infected individuals or exposure to bodily fluids. It is important to note that CMV can be present in an individual's body without causing any symptoms or illness, making detecting and preventing transmission challenging.

How Common is CMV?
The CDC states that nearly 1 in 3 children have already been infected with CMV by age 5, and by the age of 40, over half of the population is infected. The prevalence of CMV in sperm donors varies depending on the screened population. Studies have shown that CMV infection rates among sperm donors range from 30% to 70%. However, it is essential to note that the presence of CMV does not necessarily indicate active infection or the potential for transmission. Donor screening protocols typically include testing for CMV antibodies, which can help determine if the donor has contacted the virus in the past.
Symptoms of CMV Infection
CMV infection can manifest differently in individuals depending on their immune system and overall health. Many people infected with CMV may not experience symptoms or only have mild symptoms that resolve independently. However, those with weakened immune systems, such as individuals with HIV/AIDS or undergoing organ transplantation, may develop severe complications. These can include pneumonia, hepatitis, retinitis (inflammation of the retina), and neurological disorders. Awareness of these symptoms and seeking medical attention if necessary is crucial.
Becoming Infected With CMV
Primary CMV infection occurs in people who have never been exposed to the CMV virus before. Once a person becomes infected with CMV, the virus remains alive but dormant inside their body for the rest of their life. Recurrent CMV infection is when a dormant virus becomes active again. CMV infection is usually harmless and rarely causes illness. However, primary CMV infection can cause more severe problems for pregnant women than recurrent CMV infection.
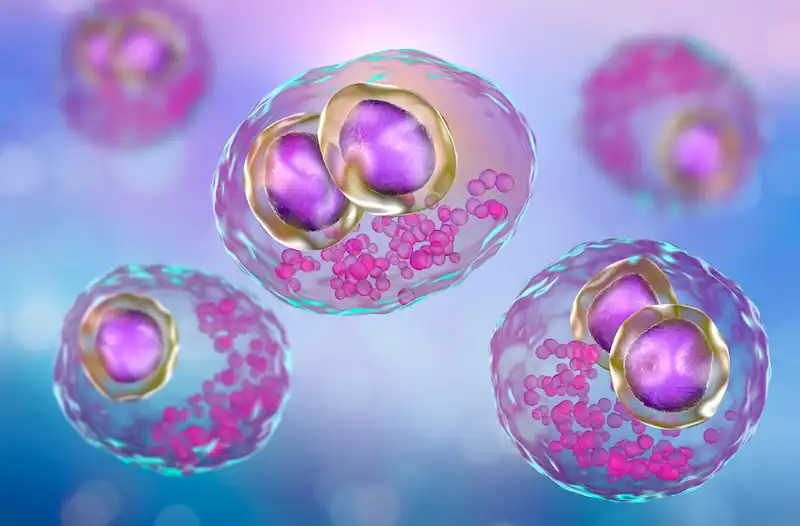
Cytomegalovirus
CMV in human cells.
Diagnosis and Treatment of CMV Infection
Diagnosing CMV infection involves various methods, including blood tests to detect the presence of CMV antibodies or viral DNA. Other tests like urine or saliva samples may also confirm active infection. Treatment options for CMV infection depend on the severity of symptoms and the individual's immune status. A healthcare provider may prescribe antiviral medications to manage the condition and reduce the risk of complications.
Prevention of CMV Transmission in Sperm Donation
Preventing CMV transmission in sperm donation involves following proper protocols and procedures. Donor screening for CMV antibodies is essential in identifying potential donors who may pose a higher risk of transmission. Additionally, implementing strict guidelines for handling and processing donated sperm can help minimize the risk of contamination. Cryopreservation techniques, such as freezing and quarantine periods, can also be employed to ensure that donated sperm is free from infectious agents before use.
CMV Protocols At Cryobank America
The FDA requires CMV testing on all men who intend to donate sperm. A positive result, however, doesn't necessarily mean that a man will be ineligible to donate. Cryobank America will obtain semen samples from potential donors and then quarantine those specimens for at least six months. During that time, the donor may have had CMV antibody levels tested several times. If the antibody tests indicate the possibility of a CMV infection close to the time of the sperm donation, the donor will not be allowed to donate their specimens. If the testing demonstrates inconclusive results, the donor will not be permitted to donate. However, if a donor tests positive for CMV IgG only, indicating a past infection, he will be eligible to contribute. These samples appear in the Cryobank America donor database as CMV-positive.
Can Washed Donor Sperm Transmit CMV?
No, clinically washed sperm is typically free from CMV (Cytomegalovirus) transmission. The sperm-washing process separates sperm from the seminal fluid, which reduces the risk of transmitting infections such as CMV. However, no medical procedure can guarantee 100% elimination of all viruses or infections. You should always consult a healthcare professional for personalized advice and information.
Considering Pregnancy Through Donor Sperm?
Women considering pregnancy with donor sperm should have CMV antibody testing as part of their IDT. Those with a past infection are at low risk of transmitting CMV infection to a fetus and are at little to no risk if they decide to use a CMV-positive donor.
Women never exposed to CMV should consider using a CMV-negative donor. Even though the risk from a CMV-positive donor is low, it is impossible to determine whether there will be a risk for infection.
Cryobank America's donor catalog has a CMV search filter for positive and negative sperm donors. To find a CMV-negative sperm donor, select negative under the CMV option!
CMV Resources
For additional information on CMV, this link is especially helpful:
https://www.mayoclinic.org/diseases-conditions/cmv/symptoms-causes/syc-20355358
If you have any questions about CMV, please email us at [email protected] or call 817-945-8708; we will be happy to help!
One fascinating aspect of artificial insemination is its potential to result in twins. Twins occur when two embryos implant in the uterus and develop simultaneously. Having twins can happen naturally, but artificial insemination can also increase the likelihood of twins due to the controlled introduction of sperm and the manipulation of the woman's reproductive system.
Key Takeaways
- The likelihood of having twins with artificial insemination is higher than natural conception.
- Age significantly affects the chances of having twins with artificial insemination.
- Fertility treatments increase the odds of having twins, with some treatments having higher rates than others.
- Multiple births with artificial insemination could come with risks and complications.
- Preparing for and coping with a twin pregnancy requires planning and management, but resources and support are available.
What are the Chances of Having Twins with Artificial Insemination?
When it comes to the chances of having twins with artificial insemination, statistics show that the likelihood is higher compared to natural conception. According to research, the rate of twin pregnancies with artificial insemination is around 10-30%, depending on various factors such as age and fertility treatments used.
In comparison, the natural occurrence of twins in the general population is approximately 1-2%. This significant difference in rates highlights how artificial insemination can significantly increase the chances of having twins for couples who desire multiple pregnancies.
Factors that Affect the Likelihood of Having Twins with Artificial Insemination
Several factors can influence the likelihood of having twins with artificial insemination. One crucial factor is age. As women age, their chances of naturally conceiving twins decrease. However, with artificial insemination, older women may still have an elevated chance of having twins due to the controlled introduction of sperm and fertility treatments.
Genetics and fertility treatments also increase the odds of conceiving multiples. Some individuals may have a genetic predisposition to releasing multiple eggs during ovulation, increasing their chances of conceiving twins. Additionally, specific fertility treatments, such as in vitro fertilization (IVF), can involve the transfer of multiple embryos, further increasing the likelihood of twins.
Age and Twin Pregnancy: How Age Affects the Chances of Having Twins
| Age Range | Chances of Having Twins | Factors That Increase Chances |
| Under 20 | 1.5% | Family history of twins |
| 20-24 | 1.8% | Family history of twins, taking fertility drugs |
| 25-29 | 2% | Family history of twins, taking fertility drugs |
| 30-34 | 1.9% | Family history of twins, taking fertility drugs |
| 35-39 | 2.3% | Family history of twins, taking fertility drugs, having had multiple pregnancies |
| 40 and Over | 3.5% | Family history of twins, taking fertility drugs, having had multiple pregnancies |
Age significantly contributes to the likelihood of having twins with artificial insemination. Women in their 30s and 40s have higher odds of conceiving twins compared to younger women. This statistic is because older women tend to have more elevated follicle-stimulating hormone (FSH) levels, which can stimulate the ovaries, prompting them to release multiple eggs during ovulation.
However, it's important to note that advanced maternal age also comes with increased risks and complications during pregnancy. Women considering artificial insemination should consult with their healthcare providers, fertility specialists, or OBG-YN to understand the potential risks associated with twin pregnancies at different ages.

Fertility Treatments and Twin Pregnancy: How Fertility Treatments Increase the Chances of Having Twins
Fertility treatments can greatly increase the chances of having twins with artificial insemination. These treatments aim to stimulate the ovaries to produce multiple eggs, increasing the likelihood of fertilization and implantation.
One standard fertility treatment that can result in twins is in vitro fertilization (IVF). During IVF, many embryos are created in a laboratory setting and then transferred into the woman's uterus. Transferring multiple embryos provides a better chance of at least one implanting successfully, potentially resulting in a twin pregnancy.
Types of Fertility Treatments and Twin Pregnancy: Which Treatments are More Likely to Result in Twins?
Different types of fertility treatments have varying rates of success when it comes to achieving a twin pregnancy. In addition to IVF, another commonly used fertility treatment is intrauterine insemination (IUI). During IUI, semen is inserted directly into the woman's uterus, increasing the chances of fertilization.
While IUI has a lower overall success rate compared to IVF, it still has the potential to result in twins. The likelihood of twins with IUI depends on factors such as the woman's age, the number of eggs she releases during ovulation, and the quality of the sperm used.
Multiple Births and Artificial Insemination: Risks and Complications
Although the idea of conceiving twins via artificial insemination may seem thrilling, it is crucial to acknowledge the potential hazards and complexities that come with multiple births. Twin pregnancies are classified as high-risk pregnancies due to the added pressure on the mother's physical well-being and the likelihood of complications.
Twin pregnancies come with a set of potential risks, such as premature births, low birth weight, gestational diabetes, preeclampsia, and placental abnormalities. Therefore, it is of utmost importance for women carrying twins to receive consistent prenatal care and monitoring to gain assurance of the health and well-being of both the mother and babies.
Preparing for a Twin Pregnancy: What to Expect and How to Plan
Preparing for a twin pregnancy requires careful consideration and planning. Expectant parents should educate themselves about the unique challenges of carrying twins and adjust their lifestyle and home environment.
A critical aspect of preparation is ensuring adequate prenatal care. Regular check-ups with healthcare providers will help monitor the status of the pregnancy and address any potential complications early on. Additionally, expectant parents may need to modify their living space, such as purchasing double strollers, cribs, and other essential items for two babies.
Coping with a Twin Pregnancy: Tips for Managing the Challenges
Managing the challenges of a twin pregnancy can be physically and emotionally demanding. Expectant mothers may experience increased fatigue, discomfort, and hormonal changes compared to singleton pregnancies.
Establishing a support network can provide invaluable assistance during this time. Joining twin support groups or online forums designed for parents of multiples can offer a sense of community through shared experiences and advice. Additionally, welcoming professional counseling or therapy can help expectant parents navigate the emotional challenges that may arise during a twin pregnancy.

Understanding the Odds and Making Informed Decisions
Artificial insemination offers couples the opportunity to conceive and experience the joy of parenthood. While the chances of having twins with artificial insemination are higher compared to natural conception, it's essential to consider individual factors such as age, genetics, and fertility treatments when assessing the likelihood of multiple pregnancies.
By understanding the science behind artificial insemination and the factors that influence twin pregnancies, couples can make informed decisions about their reproductive journey. Consulting with healthcare providers, seeking support from resources, and prioritizing self-care are all crucial steps in navigating the challenges and joys of a twin pregnancy.
Resources for Further Information and Support
Various resources are available for further information and support regarding artificial insemination, twin pregnancies, and parenting multiples. Support groups like the Twins Trust and online forums like Twins Magazine provide valuable information, advice, and a platform for connecting with other parents of multiples.
Additionally, healthcare providers specializing in fertility treatments can offer personalized guidance and support throughout the journey. It's important for couples considering artificial insemination or currently carrying twins to access these resources to gain knowledge, find support, and make informed decisions based on their unique circumstances. If you have any questions regarding your chances of having twins with artificial insemination, don't hesitate to contact Cryobank America.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Choosing IUI, ICSI, or At-Home Insemination Over IVF: 4 Factors You Should Know
Exploring different fertility treatment options requires a deep understanding of various factors, ranging from medical to financial, to personal preferences. While In-Vitro Fertilization (IVF) is undoubtedly one of the most recognized fertility treatments, other methods like Intrauterine Insemination (IUI), Intracytoplasmic Sperm Injection (ICSI), and at-home insemination have their unique appeal and benefits. But what drives the decision to choose one over the other? Here, we delve into the reasons.
1. Choosing IVF For Fertility Health and Specific Challenges
The first and foremost consideration is the specific fertility challenge a couple or individual is facing. While IVF is robust and addresses a wide array of fertility issues, some challenges may be addressed more directly with other treatments.
Male Infertility Issues
ICSI, a specialized form of IVF, has emerged as a game-changer for couples dealing with male infertility. By directly injecting a single healthy sperm into an egg, it bypasses challenges like low sperm count or poor sperm mobility. Thus, for those who have identified male infertility as the primary obstacle, ICSI might be a more direct solution than traditional IVF.
Uncomplicated Infertility Or Use Of Donor Sperm
For women with open fallopian tubes, regular ovulation, and no apparent severe infertility issues, IUI provides a less invasive approach. It's particularly popular among single women or lesbian couples using donor sperm.
2. Choosing IUI Or At-Home Insemination Due To Financial Considerations
Fertility treatments can be expensive, and not everyone has the luxury of unlimited resources or comprehensive insurance coverage.
Which Procedure Is Less Expensive, IUI or IVF?
Generally, IUI is less expensive than IVF or ICSI. For those who are on a tighter budget, starting with IUI might be a feasible first step. If several IUI cycles don't result in pregnancy, they might then consider investing in IVF or ICSI.
Cumulative Costs — What's Really More Expensive, IUI or IVF?
It's also essential to consider cumulative costs. While IUI per cycle might be cheaper, if multiple cycles are needed, the costs can add up. In contrast, IVF, though pricier upfront, might offer a higher success rate per cycle. The bottom line will be determined by your overall fertility health, donor or partner compatibility, and timing insemination correctly by precisely tracking your ovulation cycle.
Many cryobanks offer financial services such as payment plans and financing. Cryobank America has partnered with Future Family to offer patients affordable financing options.

3. Choosing IUI, IVF, or At-Home Insemination For Personal Preferences and Comfort
Medical procedures, even if they're routine from a clinical perspective, are deeply personal experiences.
Invasiveness and Comfort — IUI
IUI stands distinct with its simplicity. By directly introducing sperm into the uterus, it bypasses many of the steps intrinsic to IVF, such as egg retrieval and external fertilization. This straightforwardness can be less daunting for those who are apprehensive about medical procedures. The very nature of IUI, being less invasive, can also mean reduced physical discomfort, fewer side effects, and a shorter recovery period.
For many, starting with IUI is a gentle introduction to fertility treatments. The rationale often revolves around giving the less invasive method a try first, hoping it might lead to successful conception without the need for more complex procedures.
Natural Conception
Fertility treatments, for all their medical advancements, can sometimes feel clinical and detached from the intimate experience of conception. This feeling can be a significant determinant in the choices couples make. There's an inherent appeal in procedures that mimic or come close to the process of natural conception.
IUI, especially when executed without the aid of fertility drugs, offers an experience that's remarkably close to natural conception. The process aligns with the body's natural ovulation cycle, and the sperm is introduced directly into the uterus without any external fertilization. This method provides couples with a sense of familiarity and naturalness, making the journey feel less 'medical' and more intimate.
At-Home Insemination
The appeal of at-home insemination lies in its intimacy and privacy. For those who find clinical settings stressful or impersonal, at-home insemination offers a more comfortable and familiar environment. This method is also more cost-effective than clinical procedures, though it may have a lower success rate and lacks the oversight and expertise of a medical setting.
4. Treatment Duration and Timelines
For some, the time it takes from starting treatment to achieving pregnancy is a significant factor.
Which Procedure Is Quicker, IUI or IVF?
IUI stands out as a relatively quicker procedure when juxtaposed against IVF (in vitro fertilization). The simplicity of IUI, which involves directly introducing sperm into the uterus, eliminates several steps intrinsic to the IVF process, such as egg retrieval and lab fertilization. For those already navigating the emotionally charged waters of fertility challenges, the shorter treatment duration of IUI can be a breath of fresh air. It offers hope without the extended commitment, making it an attractive choice for those wary of prolonged medical interventions.
Does IUI or IVF Have A Higher Success Rate?
Time considerations in fertility treatments aren't just about the procedure's speed. It's also about effectiveness across multiple cycles. Here's where the dynamics become intricate. IVF, despite its lengthier process, often touts a higher success rate per cycle when compared to IUI. This statistic can translate to fewer overall treatment cycles, potentially shortening the entire duration from the start of treatment to conception.
On the flip side, the non-invasiveness, simplicity, and lower immediate costs of IUI can lead some to opt for multiple IUI cycles before considering the switch to IVF. The thought process here hinges on hope: the hope that the next IUI cycle might be a successful one, coupled with the procedure's relative simplicity.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Comparing IVF, ICSI, and IUI: Understanding Your Options in Fertility Treatments
Embarking on the path to parenthood, many couples and individuals find themselves at the crossroads of fertility treatments. The journey, while filled with hope, often presents a maze of medical terms, techniques, and decisions. The options — IVF, ICSI, and IUI — though different, all aim to assist in the realization of the dream of having a child. Delving deeper into each method helps demystify the process and sheds light on the complications involved.
Please make sure to also contact a suitable health professional. While this article is your information guide, it is not to be used as a substitute for medical opinion or healthcare treatment.
IVF (In-Vitro Fertilization)
IVF involves stimulating the ovaries using fertility drugs to produce mature eggs. These eggs are then retrieved and fertilized in a lab with sperm from a partner or a donor. The resultant embryo is monitored for signs of fertilization, and the best-quality embryo is transferred to the uterus.
Advantages of IVF
IVF is a comprehensive treatment that can address both male and female infertility factors. Through IVF, mature eggs are retrieved and fertilized in a laboratory setting, and the best-quality embryos are chosen for transfer, increasing the chances of success. The process allows for advanced embryo selection techniques, such as time-lapse monitoring and Preimplantation Genetic Screening. This ensures only embryos with the highest potential are selected. IVF provides the flexibility to use either a partner's or a donor's sperm, giving diverse options for family planning. Additionally, if more than one high-quality embryo results from the cycle, the extra embryos can be frozen for future use.
When is IVF advised?
IVF is typically recommended for those with fallopian tube damage, blockages, or in cases of unexplained infertility. It's also a viable option in mild cases of male infertility.
ICSI (Intracytoplasmic Sperm Injection)
ICSI (Intracytoplasmic Sperm Injection), on the other hand, is a refined version of IVF. Instead of allowing sperm to fertilize the egg naturally in a dish, ICSI involves the direct injection of a single, chosen sperm into the egg. This technique proves invaluable, especially in cases where male infertility is a concern. By bypassing many natural challenges, ICSI offers a chance even when sperm count is low or mobility is compromised.

Advantages of ICSI
ICSI is a specialized form of IVF where a single, healthy sperm is injected directly into the egg. This direct approach maximizes the chance of fertilization, especially in cases of male infertility. Since only the best quality sperm is selected and used, it ensures the highest potential for successful fertilization. ICSI is particularly beneficial when there are significant sperm problems, such as a low sperm count, poor sperm mobility, or high levels of DNA damage in the sperm. Even when sperm needs to be surgically retrieved, ICSI can still be applied. By addressing male fertility issues directly, ICSI bypasses many obstacles that can prevent natural fertilization.
When is ICSI advised?
ICSI is commonly prescribed for those with male fertility problems such as low sperm count, poor sperm mobility, or high levels of DNA damage in sperm. If male fertility isn't the primary issue, IVF is usually the suggested method.
IUI (Intrauterine Insemination)
IUI (Intrauterine Insemination) stands apart from the aforementioned methods. It is less invasive and mirrors the process of natural conception more closely. In this procedure, prepared sperm is directly introduced into the uterus, timed with ovulation, to facilitate fertilization. For many, IUI serves as a starting point in their fertility journey, especially when the primary concern is not related to sperm quality or quantity.
Advantages of IUI
IUI is a straightforward, non-invasive procedure without the need for anesthesia. It's generally more affordable than advanced fertility treatments such as IVF or ICSI. The entire IUI process can be completed within minutes, making it a quick and hassle-free option. The sperm "washing" process ensures that only the best and healthiest sperm are used for insemination. The timing of the insemination is carefully synchronized with the woman's ovulation to increase the chances of success. IUI can effectively address a range of infertility issues, from unexplained infertility to mild male factor problems. It's also a preferred method when using donor sperm, offering a simpler path for diverse family planning. Unlike some other treatments, there's no need for egg retrieval or surgical intervention, making it less physically demanding.
When is IUI advised?
IUI is an option for patients requiring donor sperm. To succeed, it requires clear fallopian tubes, a healthy sperm count, and a mature egg. In cases of irregular ovulation, fertility drugs may be combined with IUI.
Which Treatment is Right for You?
Your unique fertility situation will determine the best treatment. A comprehensive assessment considering your medical history, age, and response to previous treatments is necessary. For some, IUI might be the first step. However, if significant sperm disorders are detected, IVF or ICSI might be more suitable.
It's essential to understand that your fertility journey is individual. The goal is to achieve pregnancy in the most efficient and effective manner. Always ensure that you are part of the decision-making process, aware of the costs, and fully informed about the treatment path ahead.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Learn All About Christie Murphy's IUI Pregnancy Journey In This Exclusive Cryobank America Interview
When Christie Murphy and Jamie crossed paths ten years ago, little did they know that their encounter would lead to an extraordinary lifelong journey. During the aftermath of the 2020 pandemic, a mutual friend played matchmaker, sensing the potential for a deep connection between the two. And oh, how right they were!
Reflecting on that magical moment, Christie Murphy reminisces, "As cliché as it may sound, it was truly love at first sight"!

Christie Murphy with her wife, Jamie.
June 15, 2021: christie.murph wrote, "Impossible not to smile witchuuu 🧀"
Magic Beneath The Eiffel Tower: Christie Murphy Says, "I Do"
From that moment on, their lives became intertwined, inseparable in their new romance. In August of 2021, Jamie decided to take their relationship to new heights. In a picturesque outdoor setting adorned with vibrant flowers beneath the iconic Eiffel Tower, Jamie got down on one knee and proposed to Christie. Joy and excitement flooded social media as friends and family shared congratulations and well wishes for their bright future together.

Jamie proposed to Christie in Paris in August 2021
August 23, 2021: christie.murph wrote, "Haven’t yet woken up from this dream. Engaged to the LOVE OF MY LIFE in Paris! 💍"

Christie Murphy and Jamie are officially engaged.
February 14, 2022: christie.murph wrote, "Never in my WILDEST dreams did I think I’d find someone half as perfect as you; my delicious chocolate truffle 💝 #Valentine"
The Big Day
April 2022 marked a new chapter in Christie and Jamie's love story. On a sandy beach surrounded by lush palm trees, they exchanged vows in front of loved ones. Christie and Jamie looked radiant in their stunning white wedding gowns, perfectly complementing the serene backdrop.

Sharing her thoughts on marriage, Christie took to Instagram to express her gratitude:
"I still can't believe I was a BRIDE! Honestly, I never envisioned myself as a bride growing up; NEVER. Most little girls dream about it, plan their fantasy wedding, picture their dream dress, and spend hours and days daydreaming about their 'someday.' Me? NEVER. I'm unsure if it was because I never pictured myself marrying a man, or maybe I couldn't picture myself in the big white dress. Maybe I didn't find myself worthy of being a bride like I didn't feel girly enough."
Christie Murphy
"It's unbelievable, though; one day, out of nowhere, once I had grown up (and I mean grown up, into a confident, enlightened, and secure woman), I felt this sudden urge to get married and BE that bride I was once so emotionally detached from. I'm unsure if it's because I met "the one" or because I finally felt comfortable and safe enough to get married. All I know is that once I felt it, I couldn't reverse it. I pictured my dress, my flowers, my hair, my veil, my bride-to-be, her dress, her smile, ALL OF IT."

Christie Murphy On Family Planning
When we sat down with Christie and Jamie to discuss their decision to have children, their perspectives on parenthood were intriguingly different. Christie admitted that she never thought she needed to be a mother, but she was open to the idea. She explained, "I never really had that 'pull' to be a mom. I only started craving a baby after falling in love with Jamie." On the other hand, Jamie had always known that she wanted to have kids, a dream she had cherished since childhood.

Six months before the couple married, Christie and Jamie held Modern Fertility's TTC bundle with their fur babies.
October 6, 2021 christie.murph wrote, "Yes, we have our fur-babies, but Jamie & I talk about having REAL babies constantly! We’re getting married in 6 months, so we’ve already started prepping for our fertility journey with @modernfertility 🤰🏼💞🤰🏼"
Christie Murphy and her Wife, Jamie, Begin Their Donor Search
Not wasting any time, Christie and Jamie embarked on a search for the perfect sperm donor. Their quest took them across the country as they meticulously sifted through hundreds of donor profiles. In an exclusive interview, Christie shared their journey with us.
"We had specific criteria in mind, " Christie explained. "We wanted someone tall and European, with light eyes, because Jamie and I have light eyes. Resembling our families was important to us. We hoped for an athletic donor since Jamie played soccer her whole life, and I wanted him to be a brainiac."
"Finding him couldn't have been possible without Cryobank America," she said gratefully.
"Their professionalism, compassion, and unwavering support made the process smooth and stress-free. They were always there for us whenever we needed assistance, and I can't say enough great things about them".
September 21, 2022
Christie Murphy shares how she and her wife, Jamie, found their perfect donor.
After browsing through countless profiles, Christie and Jamie stumbled upon a donor who seemed tailor-made for them. A biomedical engineer with a passion for soccer and volleyball, he possessed all the qualities they sought. Cryobank America provided an audio recording, additional photos, and a handwritten letter, which allowed the couple to delve deeper into his life story, fostering an emotional connection that solidified their decision.
Christie and Jamie's IUI Pregnancy Journey Begins!
Christie and Jamie purchased Premium IUI vials, which acquire the highest concentration of motile sperm cells per milliliter. They purchased enough vials to try insemination multiple times while having the option to store extra vials for future siblings. To increase their chances of success, Christie diligently tracked her ovulation cycle using over-the-counter ovulation tests, such as Clear Blue Advanced Digital and Modern Fertility's TTC Bundle from Amazon, which detects a rise in luteinizing hormone (LH) in the urine. She gained a true sense of her peak fertile days by utilizing these resources for a few consecutive cycles.
When asked if she has any fertility tips, Christie enthusiastically shared her belief in the power of sea moss gel.
"I swear I always say sea moss got me pregnant! I took sea moss gel daily for a few weeks before we conceived. I continued to take it throughout the entire process, and I'm convinced it helped"!
Home Insemination vs. In-Clinic IUI Procedure
Christie and Jamie opted for an intimate experience in their own home using one of Cryobank America's at-home insemination kits for their first insemination attempt. However, after not achieving pregnancy on their second try, they decided it would be best to have their OB-GYN perform intrauterine insemination (IUI) within his clinic to avoid wasting any vials.
Although not mandatory, Christie's OBGYN suggested taking a follicle-stimulating hormone to maximize the chances of timely and successful ovulation. While there was a slightly increased chance of conceiving multiples, Christie trusted her OB-GYN's recommendation and decided to proceed with this fertility-boosting option. She experienced no side effects from the medication but produced three follicles that cycle and ovulated all three eggs.
Reflecting on their IUI experience, Christie emphasized the importance of trust in your fertility specialist or OB-GYN.
"I think a big factor was trusting our doctor and having a good relationship with his entire team. Our doctor even let Jamie assist him in the procedure, and we were so grateful for this!"
Overall, their IUI journey was seamless, thanks to the strong relationship they had built with their medical team.
Christie Murphy's IUI Success: Christie and Jamie Share Their Pregnancy With Family
When asked about their reaction upon seeing a positive pregnancy test, Christie couldn't contain her excitement.
"We were extremely excited and even slightly shocked because we took our test prematurely, at only nine days past ovulation! The pregnancy test looked like a strong BFN (big fat negative) until a few minutes later! We thought our eyes were deceiving themselves because it seemed almost too good to be true! We sobbed tears of joy. Sure enough, those test indicators grew darker each day!"

Christie Murphy shares her wonderful miracle.
September 12, 2023: christie.murph wrote, "I don’t think I’ll ever get over what’s going on inside my body; Miracles ✨"
The couple decided to wait until they heard a heartbeat to share the news with their immediate family. They finally revealed that they were expecting a baby at around six weeks. Little did their loved ones know, they were in for an even bigger surprise.
Christie and Jamie's Gender Reveal: Plot Twist!
On August 31, 2023, the newlyweds revealed that they wouldn't expect one baby but are expecting two bundles of joy! One by one, Christie and Jamie blasted their gender reveal cannons. Both cannons were pink, indicating Christie was carrying two twin girls!

Christie and Jamie documented their gender reveal party on Instagram, sharing pictures and videos that captured this highly anticipated moment.
September 2, 2023: christie.murph wrote, "“THE REVEAL” - aka the day we shocked our entire family 🥹"
Donor Conception
In the cryobank community, one topic that often arises is determining the best approach to discussing donor conception with your donor-conceived child. It can be a sensitive subject for some, but Christie and Jamie are open to sharing their thoughts on discussing this with their twin girls someday.
"We don't have a concrete plan for communicating with our girls about donor conception yet," Christie says. "But one thing is for sure - we won't hide anything from them or keep any secrets. We believe in full transparency and honesty."
Christie and Jamie plan on waiting until their girls are old enough to fully understand the concept of donor conception before sharing the specific details and logistics. They want to ensure their daughters have the maturity and understanding to process this information.
"We won't tell them that the stork delivered them to our doorstep," Christie adds. "But we will save the specific details for when they are a bit older and can fully comprehend how they were conceived."
We Asked Christie If There Were Anything She Would Change
When asked if there were anything they would do differently throughout their pregnancy journey, Christie reflected on their decision to try conceiving at home.
"Honestly, we wouldn't do anything differently. We do wish we didn't waste vials through at-home insemination. While it was a memorable experience filled with privacy and intimacy, we now realize we had a greater chance for success with professional assistance."
Ultimately, every couple's pregnancy journey is unique, and what works for one may not work for another. It is essential to approach the process with an open mind, realistic expectations, and a willingness to seek professional help.

Christie and Jamie hold ultrasound photos of their twin girls.
August 31, 2023: christie.murph wrote, "Marrying one another was the easiest decision we ever made; choosing to start a family was even EASIER. So much MORE love - COMING 2024 🍼"
Christie Murphy Shares Words Of Encouragement
With unwavering determination, Christie offers words of encouragement to those wishing to conceive through donor insemination. She emphasizes the uniqueness and specialness of each individual's journey towards motherhood.
"If you are someone who is trying to conceive using a sperm donor, just know that your journey to becoming a mom is so unique and so special! What is meant to happen will happen! Having trust in the journey is key! Remember to have patience, try to rely on your support system when needed, and have faith that every step of this journey will be worth it and offer so much more than you could ever imagine!"
Christie Murphy
Cryobank America Gives Special Thanks To Christie and Jamie!
Christie and Jamie's story is a testament to the power of honesty, trust, and community in navigating the path to donor conception. Their openness and willingness to share their experiences provide comfort and guidance for others embarking on this life-changing adventure. As the cryobank community grows, stories like Christie's and Jamie's remind us of the beauty and strength of embracing all unique paths to parenthood. Cryobank America feels privileged to have been part of their conception journey!
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is ICSI and How Does it Work?
ICSI, or intracytoplasmic sperm injection, is a fertility treatment that involves the direct injection of a single sperm into an egg. This procedure is performed with in vitro fertilization (IVF). During IVF, eggs are retrieved from the woman's ovaries and fertilized with sperm in a laboratory dish. With ICSI, a single sperm is selected and injected directly into each egg, bypassing any potential barriers to fertilization.
The ICSI procedure begins with collecting eggs from the woman's ovaries. These eggs are then placed in a culture dish and examined under a microscope. A single sperm is selected and immobilized using a tiny needle. The needle injects the sperm directly into the egg. After the injection, monitoring the eggs ensures that fertilization occurs. Once fertilization is confirmed, the resulting embryos transfer to the woman's uterus.
Compared to other fertility treatments, such as IVF alone, ICSI offers a higher chance of successful fertilization. This procedure is particularly beneficial for couples who have struggled with male factor infertility, where the quality or quantity of sperm may be compromised due to various factors. ICSI can be helpful in cases where previous attempts at IVF have failed or when there are concerns about the ability of the sperm to penetrate the egg.
Who is a Candidate for ICSI?
Several factors may lead to the need for ICSI.
Male factor infertility is one of the most common reasons for considering ICSI. These factors include low sperm count, poor sperm motility, or abnormal sperm morphology. ICSI can also benefit couples who have experienced previous failed attempts at IVF or have had difficulty achieving fertilization with conventional IVF methods.
Medical Conditions and ICSI
In addition to male factor infertility, certain medical conditions may affect a couple's candidacy for ICSI. These include genetic disorders that are likely to get passed on to offspring, such as cystic fibrosis or Huntington's disease. ICSI can be used with preimplantation genetic testing to screen embryos for these conditions before being transferred to the uterus.
Age Requirements For ICSI
Age can also play a role in determining whether a couple is a good candidate for ICSI. As women age, their ovarian reserve decreases, making achieving successful fertilization and pregnancy more difficult. ICSI can help overcome some of these challenges by directly injecting sperm into the egg, increasing the chances of fertilization.
Preparing for ICSI: What to Expect
Before undergoing ICSI, couples typically have an initial consultation with a fertility specialist. During this consultation, the couple's fertility specialist will review their medical history and discuss any potential factors that may affect the success of ICSI. The fertility specialist may also order additional tests and evaluations to assess the couple's health and fertility potential.
Testing and Evaluations
Medical tests and evaluations may include blood tests to check hormone levels, ultrasounds to evaluate the woman's ovarian reserve and uterine health, and semen analysis to assess the quality and quantity of sperm. These tests will help the fertility specialist determine the most appropriate treatment plan for the couple.
Medications and Injections
In preparation for ICSI, the woman may be prescribed medications to stimulate her ovaries and promote the development of multiple eggs. These medications are generally administered through injections, and the fertility clinic will closely monitor progress and any side effects. The fertility specialist will also advise the woman to make specific lifestyle changes, such as quitting smoking, reducing alcohol consumption, and maintaining a healthy diet and exercise routine.

The ICSI Procedure: Step-by-Step
The ICSI procedure typically follows a specific timeline of events. First, the woman will undergo ovarian stimulation using medications to promote the development of multiple eggs. This step is essential to increase the chances of successful fertilization and pregnancy. During this time, the woman will be closely monitored through ultrasounds and blood tests to assess the growth and maturity of the eggs.
Once the eggs have reached the desired size and maturity, retrieval occurs through a minor surgical procedure called egg retrieval. This procedure is performed under sedation or anesthesia and involves the insertion of a needle into the ovaries to collect the eggs. The eggs are then placed in a culture dish and examined under a microscope.
Next, an embryologist selects a single sperm for each egg. The embryologist carefully examines the sperm under a microscope and chooses the healthiest and most viable sperm for injection. The selected sperm is immobilized using a tiny needle and injected directly into the egg.
After the injection, the eggs are monitored to ensure that fertilization occurs. The presence of two pronuclei confirms successful fertilization. The fertilized eggs, now called embryos, are cultured in the laboratory for a few days before being transferred to the woman's uterus.
Success Rates of ICSI: What to Expect
The success rates of ICSI can vary depending on several factors, including the age of the woman, the quality of the eggs and sperm, and the overall health of the couple. Generally, the success rates of ICSI are comparable to those of conventional IVF, but ICSI can improve your success rate.
Factors that may affect the success rates of ICSI include the woman's age and ovarian reserve. As women age, their ovarian reserve decreases, making achieving successful fertilization and pregnancy more difficult. However, ICSI can help overcome some of these challenges by directly injecting sperm into the egg, increasing the chances of fertilization.
A fertility specialist should discuss realistic expectations during the initial consultation. The fertility specialist can provide personalized guidance based on the individual or couple's circumstances and help manage expectations throughout treatment.
It is also important to note that success rates can vary between fertility clinics. When choosing a fertility clinic for ICSI, it is essential to consider the clinic's success rates and the qualifications and experience of the medical team. A qualified and experienced team can significantly increase the chances of a successful outcome.
After the Procedure: What to Expect
After the ICSI procedure, the woman will typically have a recovery period of a few days. During this time, she may experience discomfort or bloating as her body adjusts to the hormonal changes. A doctor can prescribe pain medication to help manage any discomfort.
A fertility specialist will schedule follow-up appointments to monitor the woman's progress and assess the procedure's success. These appointments may include ultrasounds and blood tests to check for pregnancy and monitor embryo development.
Emotional and psychological considerations are also necessary after the ICSI procedure. Infertility can affect an individual or couple's mental health, and it is crucial to seek support and counseling if needed. Many fertility clinics offer counseling services or can provide referrals to mental health professionals who specialize in infertility.
Alternative Fertility Treatments to Consider
While ICSI is a highly effective fertility treatment, it may not be the right option for every couple. There are several alternative treatments that couples struggling with infertility may consider.
One alternative treatment is intrauterine insemination (IUI), which involves placing sperm directly into the woman's uterus during ovulation. IUI can be a less invasive and less expensive option for couples with mild male factor infertility or unexplained infertility.
In some cases, a fertility specialist may suggest gestational surrogacy. Gestational surrogacy involves using a surrogate to carry the pregnancy for the couple or individual. This process can be an option for couples where the woman cannot carry a pregnancy due to medical reasons.
It is essential for couples and individuals to thoroughly discuss their options with a fertility specialist to determine the most appropriate treatment plan for their specific circumstances.
Choosing the Right Fertility Clinic for ICSI
Choosing the right fertility clinic for ICSI is crucial for a successful outcome. There are several factors to consider when making this decision.
First and foremost, choosing a fertility clinic with a qualified and experienced team is essential. The fertility specialists should have extensive ICSI experience and be board-certified in reproductive endocrinology and infertility.
The success rates of the fertility clinic should also be considered. The clinic should have a track record of high success rates, particularly in cases similar to the couple's specific circumstances.
The clinic's facilities and laboratory should also be state-of-the-art and equipped with the latest technology and equipment. These elements will ensure that the ICSI procedure is performed under optimal conditions.
During the initial consultation with the fertility clinic, asking questions and gathering as much information as possible is essential. This information can include questions about the clinic's success rates, the qualifications and experience of the medical team, and the specific steps and timeline of the ICSI procedure.
Choosing the right fertility clinic can significantly increase the chances of a successful outcome and provide couples with the support and guidance they need during this challenging time.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What Is IUI?
IUI (intrauterine insemination), also known as artificial insemination, is a fertility treatment that involves placing sperm directly into a woman's uterus during her fertile window. This procedure benefits individuals and couples with sperm quality or quantity deficiencies, unexplained infertility, or cervical factor infertility. Unlike IVF, which involves fertilizing the egg outside the body, IUI allows natural fertilization within the woman's body.
A good candidate for IUI is a woman with open fallopian tubes, a normal uterine cavity, a partner with sufficient sperm count and motility, or donor sperm. Couples and individuals must undergo thorough fertility testing and evaluation before proceeding with IUI to ensure it is the appropriate treatment option for their situation.
Preparing for Your First IUI Procedure
Before undergoing an IUI procedure, individuals and couples will typically consult a fertility specialist. During the first consultation, the specialist will perform a physical examination, review your medical history, and discuss any previous fertility treatments or pregnancies. The specialist may also recommend additional fertility testing to determine the cause of infertility and to assess the woman's ovarian reserve.
In preparation for an IUI procedure, lifestyle changes may be recommended by your fertility clinic to improve the chances of success. These changes may include maintaining a healthy weight, avoiding alcohol, and managing stress. Additionally, the woman may be prescribed fertility medications to stimulate the ovaries and increase the number of mature eggs available for fertilization.
What Happens During the IUI Procedure?
The IUI procedure typically occurs in the fertility clinic and does not require anesthesia. The woman will lie on an examination similar to a pelvic exam. The fertility specialist will insert a speculum into the vagina to visualize the cervix. The sperm sample, washed and concentrated to remove impurities, is inserted into the uterus using a thin catheter.
The entire procedure usually takes only a few minutes and is relatively painless. Some women may experience mild cramping or discomfort during the process, but this typically subsides quickly. After the procedure, the woman will lie down briefly to allow the sperm to swim towards the fallopian tubes.

The Role of Fertility Medications in IUI
Fertility medications are often used in conjunction with IUI to increase the chances of success. These medications stimulate the ovaries and promote the development of multiple mature eggs. The most commonly used medications in IUI are oral medications such as Clomid or letrozole, which help regulate ovulation.
In some cases, your fertility clinic may use injectable medications such as gonadotropins to stimulate the ovaries. These medications contain follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which help promote the growth and maturation of multiple eggs. In cases where oral medications have not been successful or more mature eggs are needed, your fertility specialist will use injectable medications.
While fertility medications can increase the chances of success in an IUI procedure, they come with potential side effects. These side effects may include bloating, mood swings, hot flashes, and breast tenderness. Couples must discuss their fertility medications' potential risks and benefits with their fertility specialist before starting treatment.
Potential Risks and Side Effects of IUI
Like any medical procedure, IUI carries some risks. One of the most common risks associated with IUI is the possibility of multiple pregnancies. Because fertility medications stimulate the ovaries and increase the number of mature eggs, there is a higher chance of conceiving twins or even triplets. This risk can be minimized by ensuring your fertility specialist closely monitors your response to fertility medications and adjusts the dosage if necessary.
Regarding side effects, IUI is generally a well-tolerated procedure with minimal discomfort. Some women may experience mild cramping or spotting after the procedure, but these symptoms usually subside within a day or two. Infection or damage to the uterus or fallopian tubes may occur in rare cases, but these complications are extremely rare.
Post-IUI Care and Recovery
After an IUI procedure, couples will typically receive aftercare instructions from their fertility specialist. These instructions may include recommendations for rest, avoiding strenuous activities or exercise, and refraining from sexual intercourse for a certain period. Couples need to follow these instructions to optimize their chances of success.
Most women can resume their normal daily activities after an IUI procedure. However, it is essential to listen to your body and to take it easy if you are experiencing any discomfort or pain. You should also schedule a follow-up appointment with your fertility specialist to discuss your results and determine the next steps.
Interpreting the Results of Your IUI Procedure
The results of an IUI procedure are determined through a pregnancy test, usually done about two weeks after the procedure. A positive result indicates that pregnancy has occurred, while a negative result means pregnancy has not been achieved. It is important to note that a negative result does not necessarily mean the procedure was unsuccessful, as it may take multiple attempts before achieving a successful pregnancy.
If the results of the IUI procedure are positive, it is important to schedule an appointment with an obstetrician or midwife to confirm the pregnancy and to begin prenatal care. You should consult your fertility specialist to discuss the next steps if the results are negative. These may include repeating the IUI procedure, exploring other fertility treatment options such as ICSI or IVF, or further testing to determine the cause of infertility.
What to Do If Your First IUI is Unsuccessful
If your first IUI procedure is unsuccessful, it is important to remember that you are not alone. Many couples require multiple attempts before achieving a successful pregnancy. It is important to discuss the reasons for the unsuccessful IUI with your fertility specialist and to explore other options.
Depending on the circumstances, your fertility specialist may recommend repeating the IUI procedure with or without additional fertility medications. Alternatively, they may suggest exploring other fertility treatment options, such as IVF or intracytoplasmic sperm injection (ICSI). An open and honest discussion with your fertility specialist is crucial to determining the best course of action for your situation.
Exploring Other Fertility Treatment Options
While IUI is a widely used and effective fertility treatment, it may not be the best option for every individual or couple. There are several other fertility treatment options available, including IVF and ICSI.
IVF involves fertilizing the egg outside the body and transferring the resulting embryo(s) into the uterus. ICSI is a similar procedure but involves injecting a single sperm directly into the egg.
When considering other fertility treatment options, you must consider factors such as age, overall health, and the cause of infertility. Consulting with a fertility specialist can help determine the best course of action based on individual circumstances.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
We Offer Donor Storage Options Until You're Ready!
Are you planning to use donor sperm to conceive but aren't quite ready to get pregnant? Have you stumbled upon your perfect match before deciding you're ready to conceive? We understand that timing is everything when it comes to starting a family. Whether you're waiting for the perfect moment, focusing on your career, or want to ensure that your chosen donor's sperm is available when you're ready, Cryobank America has got you covered.
We offer a comprehensive sperm storage solution designed with your needs in mind. Our state-of-the-art facility ensures your chosen donor sperm is stored safely and securely until you're ready to use it. We adhere to the strictest standards of quality control and follow rigorous protocols to maintain the integrity of our stored specimens.
Donor Sperm Storage For Future Use
Finding the perfect donor is a significant part of your journey towards parenthood. We offer a database of diverse donor profiles for you to browse at your leisure. Each profile provides detailed information about the donor, including blood type, physical characteristics, CMV status, and more. This information allows you to make an informed decision about who will be contributing half of your future child's genetic material. You can find additional information on each donor when you sign up for our Premium Membership.
Once you've found your ideal donor, securing their sperm for future use is a simple process with Cryobank America. Our experienced professionals will guide you through every step, ensuring your experience is as smooth and stress-free as possible.
Will My Donor Sperm Be As Viable After Remaining In Storage?
Our cryopreservation process ensures that donor sperm can survive many years, maintaining its viability as if you had chosen to use it immediately. This advanced technology allows us to freeze and store sperm cells at extremely low temperatures, halting their biological clock and preserving their fertilization ability.
Our cryopreserved samples' longevity means you can plan your family at your own pace without the pressure of time constraints. Whether you're considering parenthood now or in the future, our services offer you the flexibility and security you need.
Donor Sperm Storage For Future Siblings
Storing your donor's sperm with us also opens up the possibility of having future siblings from the same donor. This option can be particularly appealing for those wishing to provide their child with a biological sibling connection later. We understand the importance of these familial bonds and are proud to facilitate such possibilities through our storage services.

Choosing Cryobank America
We understand this is a big decision, and we want you to feel confident in choosing Cryobank America as your partner in this journey. That's why we offer unparalleled customer service and support throughout the process. Our dedicated team is always available to answer any questions or concerns.
So, rest assured if you've found your perfect donor but aren't quite ready to conceive yet. Cryobank America will safely store your chosen donor sperm until you're ready. Trust us with your future – because at Cryobank America, we're not just storing sperm but safeguarding dreams.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
The Average Success Rate for Artificial Insemination
Artificial insemination (AI) is a fertility treatment that involves placing sperm directly into a woman's reproductive system to increase the chances of pregnancy. It is a popular option for couples struggling with infertility or for same-sex couples who wish to conceive. The average success rate for artificial insemination ranges between 5% to 30% per cycle, and success can depend on several factors. Understanding these factors is crucial for making informed decisions about your fertility treatments.
Factors Affecting the Success Rate For Artificial Insemination
Several factors can affect the success rate of artificial insemination, including sperm quality, timing, age, and fertility drugs.
What's the most important factor? You guessed it; it's sperm quality! Healthy sperm is necessary for fertilization, and poor sperm quality can significantly reduce the chances of pregnancy. Timing is also crucial, as insemination must occur during the woman's fertile window. Age is another factor affecting success rates, as fertility declines with age. Fertility drugs are often used to stimulate ovulation and increase the chances of pregnancy. Finally, the selected method for artificial insemination can impact the outcome for success.
Understanding the Role of Sperm Quality in the Success Rate For Artificial Insemination
Sperm quality refers to the ability of sperm to fertilize an egg and produce a viable pregnancy. Various factors such as sperm count, motility, morphology, and DNA integrity determine the overall quality. High-quality sperm is essential for achieving successful pregnancies through artificial insemination. Poor sperm quality can lead to low fertility rates, reduced conception rates, and increased risk of embryonic loss.
The impact of poor sperm quality on fertility rates cannot be overstated. Women who inseminate with low-quality sperm can result in failed pregnancies or offspring with genetic abnormalities. Therefore, it is crucial to ensure that you are receiving high-quality sperm for your artificial insemination procedure.
Several factors can affect sperm quality, including environmental and genetic factors. Environmental factors such as temperature, nutrition, and stress can significantly impact sperm quality. High temperatures can damage sperm cells, while poor nutrition can lead to reduced sperm production and motility. Stress can also affect sperm quality by decreasing testosterone levels and increasing oxidative stress.
Genetic factors also play a crucial role in determining sperm quality. That's why we only accept high-quality applicants with desirable traits to improve the overall genetic quality of offspring produced through artificial insemination.
At Cryobank America, we offer premium-grade IUI vials. IUI vials are a great choice because they include sperm that has undergone a density gradient separation wash. This method purifies and isolates the healthiest cells, removing biological debris and seminal fluid, ultimately increasing your success rate. Click here to learn more about our vial types. Click here to view vial pricing.

The Importance of Timing in Artificial Insemination
Timing is crucial in achieving pregnancy through artificial insemination. The window of opportunity for successful insemination is relatively small, and missing it can significantly reduce the chances of conception. Sperm can survive in the female reproductive system for up to five days, but the egg is only viable for 12-24 hours after ovulation. Therefore, it is essential to time the introduction of sperm correctly to coincide with ovulation.
The timing of insemination can also affect the quality of sperm that reaches the egg. Sperm inside of the female reproductive system for too long may become less motile and less capable of fertilizing an egg. On the other hand, introducing sperm too early can result in a lower concentration of sperm, reducing the chances of successful fertilization.
Understanding the menstrual cycle and its phases is crucial to achieving successful insemination. The menstrual cycle is divided into three phases: follicular, ovulatory, and luteal. The follicular phase begins on the first day of menstruation and lasts until ovulation. During this phase, follicles in the ovaries mature and prepare to release an egg.
The ovulatory phase is when ovulation occurs, and an egg is released from the ovary. This phase typically lasts 24 hours but can extend up to 48 hours. Finally, during the luteal phase, the body prepares for pregnancy by thickening the uterine lining.
The timing of insemination is critical during the ovulatory phase since the egg is released from the ovary and travels down the fallopian tube. Therefore, tracking menstrual cycles can help determine when ovulation occurs and increase the chances of successful insemination.
The Impact of Age on the Success Rate For Artificial Insemination
The biological clock refers to the natural decline in fertility that occurs as women age. As women age, their eggs become less viable, and the chances of conceiving naturally or through fertility treatments decrease. This decline in fertility is due to a decrease in the number and quality of eggs available for fertilization.
Age also impacts the success rates of artificial insemination. Studies have shown that women over 35 have lower success rates with artificial insemination than younger women. Older women have fewer viable eggs and are more likely to have underlying fertility issues that can impact the success of the treatment.
Studies have shown that women under 35 have success rates of around 20% per cycle with artificial insemination; however, this success rate decreases as women age. Women over 35 have success rates of approximately 10% per cycle, and women over 40 have success rates of around 5% per cycle. Women are born with a finite number of eggs, and as they age, the number and quality of these eggs decline. When a woman reaches her mid-30s, her fertility begins to fall rapidly.
Other age-related factors impacting success rates include underlying fertility issues, such as endometriosis or polycystic ovary syndrome (PCOS), and lifestyle factors, such as smoking or obesity.
The Role of Fertility Drugs in Artificial Insemination
Fertility drugs are often used in conjunction with artificial insemination to increase the chances of pregnancy. These drugs work by stimulating ovulation and increasing the number of eggs available for fertilization.
Several fertility drugs are available, including Clomifene citrate (Clomid), Metformin, and Gonadotropins. These drugs can significantly increase the chances of pregnancy when used correctly.
Tips for Maximizing the Success of Artificial Insemination
Several lifestyle changes can help maximize the success rate of artificial insemination, including maintaining a healthy weight, reducing stress levels, and avoiding smoking and excessive alcohol consumption.
Choosing the proper fertility treatment and clinic is imperative for the best outcome. Preparing for the procedure by carefully following all instructions can also increase the chances of pregnancy. Finally, post-insemination care is crucial for ensuring a healthy pregnancy.
Advances in AI technology are continually improving success rates and making personalized treatments more accessible than ever. Understanding success rates is crucial for making informed decisions about fertility treatments and achieving a successful pregnancy.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States

