When it comes to starting a family, there are many decisions you must make. One of those decisions is choosing a sperm donor. While this may seem like a straightforward process, it is crucial to prioritize the protection of one's health. There has been increased discussion and visibility of natural insemination (NI) in recent years, mainly due to online platforms and forums that connect individuals seeking sperm donors. While some people may choose natural insemination for various reasons, you should consider this method's potential risks. Opting for a sperm bank and artificial insemination (AI) can increase safety and peace of mind.
Key Takeaways
- Natural insemination carries risks of sexually transmitted infections and unwanted pregnancies.
- Choosing a sperm bank provides quality control measures and screening/testing of donors.
- Donor anonymity and confidentiality are maintained, but recipients can access medical history and donor profiles.
- Legal protections exist for both donors and recipients in the sperm bank process.
- Artificial insemination can provide better chances of pregnancy.
- While cost and accessibility may vary, making an informed decision for your health is crucial.
What is Natural Insemination?
Natural insemination refers to the process of conceiving a child through sexual intercourse with a sperm donor. Unlike sperm banks, natural insemination involves direct contact between the donor and the recipient. While some individuals may prefer this method due to its perceived intimacy, it is essential to consider the potential risks involved.
The Risks of Natural Insemination
When it comes to natural insemination, there are several health risks that both donors and recipients should be aware of. Firstly, there is an increased risk of sexually transmitted infections (STIs) as there is direct contact between the donor and recipient. Additionally, there is a lack of quality control and screening measures in place, which can lead to potential genetic disorders or other health complications for the child.
From a legal standpoint, natural insemination poses risks for both parties. Donors may face unexpected legal responsibilities and obligations towards the child without proper legal agreements. Similarly, recipients may encounter difficulties establishing legal parentage or obtaining financial support from the donor.

The Benefits of Choosing AI Over NI
| Benefit | Assisted Hatching May Benefit: |
| Increased chances of conception | Sperm banks offer a wide selection of healthy and viable sperm, increasing the chances of successful conception. |
| Screened donors | Sperm banks thoroughly screen and test their donors for genetic and infectious diseases, ensuring the safety of the recipient and any resulting offspring. |
| Privacy and anonymity | Sperm banks offer the option to donate anonymously, allowing recipients to maintain their privacy and avoid potential legal or emotional complications. |
| Access to medical history | Sperm banks provide detailed medical histories and updated reports of their donors, allowing recipients to make informed decisions about their choice of donor and potential health risks. |
| Convenient and flexible scheduling | Sperm banks offer flexible scheduling options for donors and recipients, making sperm donation and insemination more convenient and accessible. |
Opting for a sperm bank offers numerous benefits when compared to natural insemination. Firstly, sperm banks provide increased safety and protection for donors and recipients. Sperm samples are thoroughly screened and tested for genetic disorders, infectious diseases, and other health conditions before being made available for use. This rigorous screening process significantly reduces the risk of passing on hereditary diseases or infections to the child.
Furthermore, sperm banks offer access to high-quality sperm from carefully selected donors. Donors undergo extensive screening, including medical and psychological evaluations, to ensure suitability. These screenings ensure that recipients have access to sperm from healthy individuals with desirable genetic traits, increasing the chances of a successful pregnancy.
Quality Control Measures in Sperm Banks That You Won't Get Through Natural Insemination
Sperm banks prioritize quality control measures to ensure the health and safety of recipients. The screening and testing process for sperm donors is comprehensive and stringent. Donors are required to undergo thorough medical examinations, including genetic testing, to identify any potential health risks. Additionally, they receive screenings for infectious diseases such as HIV, hepatitis, and syphilis.
Sperm samples are also subject to strict quality control measures. They are tested for motility, viability, and concentration to ensure their suitability for fertility treatments. By implementing these quality control measures, sperm banks assure recipients that they receive sperm from healthy and viable donors.
Screening and Testing of Donors
The screening and testing process for sperm donors ensures the health and well-being of recipients and their future children. Donors must undergo a series of evaluations to assess their physical and mental health. These evaluations include a comprehensive medical history review, physical examinations, and genetic testing.
Genetic testing is vital in identifying potential hereditary diseases that could affect future children. Donors receive screenings for conditions including cystic fibrosis, sickle cell anemia, and various genetic disorders. By conducting these tests, sperm banks can provide recipients with valuable information about the genetic health of their chosen donor.
Donor Anonymity and Confidentiality
Donor anonymity and confidentiality are essential considerations when choosing a sperm donor. Sperm banks prioritize the protection of donor identities to ensure their privacy. This anonymity allows donors to contribute without fear of future legal or emotional obligations towards the child.
Recipients also benefit from donor anonymity, as it allows them to make decisions about their family without external interference. It will enable them to focus on their desires and preferences when selecting a donor without feeling obligated to establish a relationship with the donor in the future.
Access to Donor Information and Medical History
One of the significant advantages of using a sperm bank is the access recipients have to comprehensive donor information and medical history. Sperm banks maintain detailed profiles for each donor, including physical characteristics, educational background, and personal interests. This information allows recipients to choose a donor who aligns with their preferences and values.
Furthermore, recipients have access to the donor's medical history. This information includes any known or newly developed genetic conditions or family health issues. This information is invaluable in understanding potential health risks for the child and making informed decisions about their future well-being.
Diversity of Donor Profiles
Sperm banks offer an extensive range of donor profiles, ensuring recipients have a diverse selection. Donors come from various ethnic backgrounds, allowing recipients to find a donor who shares their cultural heritage. Diversity is crucial for those who want to preserve their cultural roots or guarantee their offspring will inherit a varied genetic makeup.
The availability of diverse donor profiles also ensures that recipients can find donors who possess specific physical traits or talents they desire for their child. Whether it is eye color, height, or musical abilities, sperm banks provide an extensive selection to cater to individual preferences.
Legal Protections for Donors and Recipients
When using a sperm bank, both donors and recipients are protected by legal frameworks. This framework shields donors from legal responsibilities or obligations towards the child conceived through their donation. Recipients, on the other hand, are provided with legal protections regarding parentage and financial support.
These legal protections provide peace of mind for both parties involved, ensuring they can make decisions about their family without fear of future legal complications or disputes.
Cost and Accessibility of Sperm Banks
While the cost of using a sperm bank may be higher compared to natural insemination, the long-term benefits and peace of mind it provides make it worth the added costs. Sperm banks offer various pricing options, allowing recipients to choose a plan that suits their budget. Additionally, many sperm banks provide financing options to make the process more accessible.
Regarding accessibility, sperm banks have a vast network of locations, making it easier for individuals to access their services. These expansions ensure that individuals from different geographical areas have equal opportunities to choose a suitable donor and start their journey toward parenthood.
Choosing A Sperm Bank Over Natural Insemination For Your Health
Protecting one's health should be a top priority when choosing a sperm donor. While natural insemination may seem appealing due to its perceived intimacy and low costs, it comes with significant risks, both in terms of health and legality. Opting for a sperm bank provides increased safety and protection for both donors and recipients.
Sperm banks implement rigorous quality control measures, including comprehensive screening and testing processes for donors. Testing ensures recipients access high-quality sperm from healthy individuals with desirable genetic traits. Additionally, sperm banks offer valuable donor information and updated medical history, allowing recipients to make informed decisions about their future families.
By choosing a sperm bank over natural insemination, you can ensure optimal health and safety while embarking on parenthood. Making a calculated decision that considers long-term implications and provides the best possible outcome for all parties involved is crucial.
Natural Insemination and Artificial Insemination FAQ
What is a sperm bank?
A sperm bank is a facility that collects, freezes, and stores sperm from donors for use in artificial insemination procedures, such as IUI, ICI, IVF, ICSI, and home insemination.
What are the benefits of choosing a sperm bank over natural insemination?
Choosing a sperm bank over natural insemination can provide several benefits. These benefits include access to a wide range of donors, increased control over the selection process, and reduced risk of sexually transmitted infections and passing on genetic conditions.
Does natural insemination have a higher success rate than artificial insemination?
No scientific evidence suggests that natural insemination's success rate is higher than artificial insemination. Artificial insemination techniques have been developed and refined over many years to maximize the chances of successful conception. They allow for controlled and precise placement of sperm, which can increase the likelihood of fertilization.
Is using a sperm bank more expensive than natural insemination?
The cost of natural insemination can vary depending on the donor and the specific arrangement. Some NI donors may offer their services for free, while others may charge a fee. Using a sperm bank can be expensive, with costs ranging from $500 to $10,000 per cycle. However, many insurance plans cover the costs of fertility treatments, and many sperm banks offer financing options.
Can I choose the physical characteristics of the sperm donor?
Many sperm banks provide childhood and adult photos of each donor, allowing recipients to select donors based on physical characteristics. They also offer photo-matching services so recipients can choose a donor that closely resembles their physical traits.
Is using a sperm bank safe?
Using a reputable sperm bank is safe. They are regulated and inspected by the Food and Drug Administration (FDA) and Clinical Laboratory Improvement Amendments (CLIA) to ensure optimal safety. Additionally, sperm is stored and handled in a controlled environment to prevent the risk of contamination or infection.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
In vitro fertilization (IVF) is a widely used assisted reproductive technique that has assisted many couples in achieving pregnancy. The success rates of IVF have improved significantly over the years. However, there are still cases where the embryos are unable to implant in the uterus, resulting in unsuccessful pregnancies, which is where assisted hatching comes into play.
Assisted hatching is a new technique that aims to improve IVF's success rates by opening or thinning the embryo's outer shell (zona pellucida) before uterine transfer. This procedure allows for easier implantation and increases the chances of a successful pregnancy.
Key Takeaways
- Assisted hatching is a technique implemented in IVF to help embryos hatch from their protective outer layer.
- This technique may benefit couples who have had multiple failed IVF attempts or who have poor embryo quality.
- Assisted hatching carries a few risks, including potential damage to the embryo and increasing the chance of multiple pregnancies.
- The success rates of assisted hatching vary depending on the individual case and the clinic performing the procedure.
- Assisted Hatching may not be necessary for everyone.
- Alternatives to assisted hatching include natural hatching, blastocyst transfer, and pre-implantation genetic testing.
Understanding the IVF Process
Before delving deeper into assisted hatching, we'll cover how IVF works and why embryo quality plays a crucial role in its success. The process begins with ovarian stimulation, where you'll receive fertility medications to stimulate egg production. The produced eggs are then retrieved and fertilized with sperm in a laboratory.
Once fertilization occurs, embryos start developing over several days under carefully controlled conditions. During this time, embryologists closely monitor their growth and quality before selecting one or more embryos for transfer into the woman's uterus.
Embryo quality is vital because only high-quality embryos have better chances of implanting successfully and developing into healthy pregnancies. However, even with good-quality embryos, there can be instances where they fail to attach themselves firmly to the uterine lining due to various factors such as thick zona pellucida or poor embryo development.
What is Assisted Hatching?
Assisted hatching involves creating an opening or thinning out the zona pellucida using specialized techniques before transferring an embryo during an IVF cycle. This procedure helps facilitate embryo implantation by making it easier for them to break through this protective layer and attach to the uterine lining.
Different methods for assisted hatching include mechanical, chemical, or laser-assisted techniques. Mechanical methods involve using a microtool to create a small hole in the zona pellucida, while chemical methods use acidic solutions to dissolve part of it. Laser-assisted hatching utilizes laser technology to thin out the zona pellucida precisely.
By performing assisted hatching, fertility specialists aim to enhance embryo implantation rates and increase the chances of pregnancy for individuals undergoing IVF treatment.

Who Can Benefit from Assisted Hatching?
| Assisted Hatching May Benefit: | |
| ✔️ | Women over the age of 38 |
| ✔️ | Women with a high FSH level |
| ✔️ | Women with a history of failed IVF cycles |
| ✔️ | Women with thick zona pellucida |
| ✔️ | Women with poor embryo quality |
Assisted hatching may be a good option for certain patients who are undergoing IVF treatment. Factors that may make someone a good candidate for assisted hatching include advanced maternal age (typically over 35), previous failed IVF cycles, thick zona pellucida observed during embryo evaluation, or poor embryo quality.
Women with reproductive conditions such as polycystic ovary syndrome (PCOS) or endometriosis may also benefit from assisted hatching due to potential difficulties in embryo implantation caused by these conditions. Additionally, patients with unexplained infertility or those who have undergone multiple unsuccessful IVF cycles despite good-quality embryos might find assisted hatching helpful.
It is important to note that not all patients will require or benefit from assisted hatching. Fertility specialists will evaluate each case and recommend this technique only when they believe it can significantly improve the chances of success.
Risks and Benefits of Assisted Hatching
As with any medical intervention, there are possible risks associated with assisted hatching that patients should be aware of before making a decision. These risks include damage to the embryo during the procedure and an increased risk of monozygotic (identical) twinning due to manipulation of the zona pellucida.
However, it's essential to weigh these risks against the potential benefits offered by assisted hatching. Studies have shown that this technique can increase embryo implantation rates by up to 50% and improve the chances of pregnancy, particularly in patients with specific conditions or circumstances that may hinder natural implantation.
By thinning or creating an opening in the zona pellucida, assisted hatching allows embryos to attach to the uterine lining more efficiently, increasing the likelihood of successful implantation and subsequent development into a healthy pregnancy.
How is Assisted Hatching Performed?
Assisted hatching occurs on day three or day five of embryo development, depending on the clinic's protocols and individual patient factors. It is performed in a laboratory setting by highly trained embryologists.
The most common method for assisted hatching involves a laser that creates an opening or thins out the zona pellucida. This laser-assisted technique offers precise control over the size and location of the opening, minimizing potential damage to the embryo.
Depending on clinic preferences and patient-specific factors, your clinic may use other methods, such as mechanical or chemical techniques. These methods involve using microtools or acidic solutions to penetrate the zona pellucida.
Success Rates of Assisted Hatching
The success rates of assisted hatching vary depending on various factors such as patient age, overall health, underlying fertility issues, and previous IVF outcomes. However, studies have shown that this technique can significantly improve IVF success rates for certain patients.
Research suggests that older patients (over 35) with thick zona pellucida observed during embryo evaluation benefit more from assisted hatching than younger patients without these conditions.
It's important to note that while assisted hatching can increase implantation rates and improve IVF outcomes for some couples, it does not guarantee success in every case. Fertility specialists will assess each situation carefully before recommending this procedure.
Do I Need Assisted Hatching During IVF?
Not all IVF cycles require assisted hatching. The decision to use assisted hatching depends on various factors related to the individual or couple undergoing IVF treatment. Here are some scenarios where assisted hatching might not be necessary:
1. Younger Women with Good Prognosis: Women under the age of 37 or those with a good ovarian reserve and high-quality embryos may not need assisted hatching, as their embryos are generally healthier and more capable of hatching on their own.
2. High-Quality Embryos: If the embryos have reached the blastocyst stage (usually by day 5 or 6 after fertilization) and are of high quality, they might not require assisted hatching. Blastocysts have already begun the hatching process naturally in many cases.
3. Previous Successful IVF without Assisted Hatching: Couples who have had successful IVF cycles without assisted hatching may not need it in subsequent cycles, assuming similar conditions and embryo quality.
4. Concerns about Potential Risks: Although rare, there are potential risks associated with assisted hatching, such as damage to the embryo or increased chances of monozygotic (identical) twins. Some couples or individuals may avoid these risks if their situation does not strongly indicate a need for assisted hatching.
5. Specific Laboratory Protocols: Some IVF clinics or laboratories may have specific protocols and criteria for when to recommend assisted hatching based on their experience and success rates. If their assessment suggests that assisted hatching is not beneficial for a particular case, it may not be necessary.
It's important to note that the decision to use assisted hatching should be made on a case-by-case basis, considering each patient's specific circumstances and medical history. Fertility specialists can provide guidance based on assessing an individual's or couple's likelihood of benefiting from this procedure.
Cost of Assisted Hatching
The cost of assisted hatching can vary depending on the fertility clinic and the specific techniques. It is typically an additional procedure that incurs extra fees on top of the standard IVF treatment expenses.
Your fertility clinic can discuss costs associated with assisted hatching and whether your insurance plan covers it. Some plans may provide coverage for this procedure, while others may consider it an elective add-on that requires out-of-pocket payment.
Alternatives to Assisted Hatching
While assisted hatching can be beneficial for certain patients, alternative techniques are available to improve embryo quality and IVF success rates. These alternatives include pre-implantation genetic testing (PGT), which involves the selection of genetically normal embryos before transfer, and embryo co-culture, where embryos are cultured alongside supportive cells in the laboratory.
Each alternative technique has pros and cons, and fertility specialists evaluate each patient's unique circumstances to determine the most suitable approach.
Choosing the Right Fertility Clinic for Assisted Hatching
When considering assisted hatching or any other fertility treatment, choosing the right fertility clinic is crucial. Factors you should consider when selecting a clinic include:
- Its experience in performing assisted hatching procedures.
- Success rates with this technique.
- Availability of specialized equipment such as lasers if laser-assisted hatching is preferred.
- Overall reputation within the field.
It's also important to ask questions during consultations with potential clinics regarding their experience in treating patients with conditions or circumstances similar to yours. Understanding their protocols will help you decide whether they can effectively handle your needs.
Frequently Asked Questions About Assisted Hatching
What is assisted hatching in IVF?
Assisted hatching is a new technique used during in vitro fertilization (IVF) to help embryos hatch from their protective outer layer, called the zona pellucida, and implant in the uterus.
How is assisted hatching performed?
Assisted hatching uses a laser or chemical solution to create a small hole in the embryo's zona pellucida.
Who might benefit from assisted hatching?
Assisted hatching may benefit couples who have had multiple failed IVF cycles, older women, or those with thick or abnormal zona pellucida.
What are the risks of assisted hatching?
There is a small risk of damaging the embryo during the assisted hatching procedure, which could result in the embryo not developing correctly or failing to implant.
What is the success rate of assisted hatching?
The success rate of assisted hatching varies depending on the individual case. Studies have shown that it may increase the chances of pregnancy and live births in certain groups of patients.
Do I need assisted hatching if I'm doing IVF?
Not all IVF cycles require assisted hatching. The decision to use assisted hatching depends on various factors related to the individual or couple undergoing IVF treatment. Assisted hatching might not be necessary if you are young and have a good prognosis, have high-quality embryos, have had a previous successful IVF without assisted hatching, or are concerned about the procedure's risks.
Is assisted hatching covered by insurance?
Assisted hatching may or may not be covered by insurance, depending on your specific policy and the reason for the procedure. Patients should always contact their insurance providers to see if they are covered.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Gynecological (GYN) surgery plays a crucial role in the journey of patients undergoing artificial insemination. It is a specialized field of surgery that focuses on the female reproductive system, addressing various conditions and improving fertility outcomes. This comprehensive article will delve into GYN surgery, its basics, its importance for artificial insemination patients, and much more.
Key Takeaways
- GYN surgery can treat a variety of conditions, including endometriosis, fibroids, and infertility.
- Understanding the risks and benefits of GYN surgery is essential for making informed decisions.
- Different artificial insemination procedures exist, including intrauterine insemination and in vitro fertilization.
- Post-operative care and recovery tips can help manage pain and discomfort after surgery.
- Success rates and long-term outcomes of artificial insemination vary depending on individual factors.
Understanding the Basics of GYN Surgery
GYN surgery refers to procedures performed on the female reproductive system. It encompasses various procedures, including hysterectomy, myomectomy, ovarian cystectomy, and tubal ligation reversal. These surgeries treat multiple conditions, such as uterine fibroids, endometriosis, ovarian cysts, and tubal blockages.
For artificial insemination patients, GYN surgery is often necessary to address underlying conditions that may hinder successful conception. Correcting these conditions through surgical intervention significantly improves the chances of achieving a successful pregnancy. GYN surgery can help optimize patients reproductive health patients reproductive health and increase their chances of conceiving through artificial insemination.
Preparing for Artificial Insemination Surgery
You should take several steps before undergoing GYN surgery for artificial insemination. It is crucial to have a thorough consultation with your doctor to discuss your medical history, current condition, and expectations from the surgery. Your doctor will give pre-operative instructions, including dietary restrictions, medication adjustments, and lifestyle modifications.
During the consultation, your doctor will conduct a physical exam and provide additional tests to assess your reproductive health. This exam will help determine your specific condition's most appropriate surgical approach. You should be open and honest with your doctor about any concerns or questions during this process.

What Conditions Can GYN Surgery Treat?
| Condition | Description |
| Uterine Fibroids | Non-cancerous uterine growths that can cause heavy bleeding, pain, and discomfort. |
| Endometriosis | A medical condition characterized by the growth of uterine tissue outside of the uterus, resulting in discomfort and reduced fertility. |
| Ovarian cysts | A condition where the ovaries develop fluid-filled sacs, which can cause pain and discomfort. |
| Abnormal Uterine Bleeding | Heavy or irregular bleeding unrelated to a menstrual cycle. |
| Pelvic Organ Prolapse | A medical condition characterized by the descent of organs such as the bladder or uterus into the vaginal region. |
| Gynecologic Cancer | Cancer within the female reproductive system, including the cervix, uterus, ovaries, and fallopian tubes. |
GYN surgery can address a wide range of conditions that may affect fertility and hinder the success of artificial insemination. Some common conditions include uterine fibroids, which are benign growths in the uterus that may interfere with implantation and pregnancy. Endometriosis, a medical condition characterized by the growth of tissue outside of the uterus, can be effectively treated through GYN surgery. Surgical interventions can treat other conditions, such as ovarian cysts and tubal blockages.
By treating these conditions, GYN surgery can significantly improve fertility outcomes for patients undergoing artificial insemination. It creates a more favorable environment for conception and increases the chances of successful pregnancy.
Understanding the Risks and Benefits of GYN Surgery
GYN surgery comes with potential risks such as infection, bleeding, harm to nearby organs, and adverse reactions to anesthesia. These risks are generally low and can be minimized by carefully choosing a reputable surgeon and following pre-operative and post-operative instructions.
On the other hand, the benefits of GYN surgery for artificial insemination patients are numerous. By addressing underlying conditions that may hinder conception, GYN surgery increases the chances of successful pregnancy through artificial insemination. It optimizes patients' reproductive health and gives them a better chance at achieving their dream of starting a family.
The Different Types of Artificial Insemination Procedures
Artificial insemination encompasses two main procedures: intrauterine insemination (IUI) and in vitro fertilization (IVF). IUI involves sperm insertion directly into the uterus during ovulation, while IVF involves fertilizing eggs with sperm in a laboratory before the resulting embryos are transferred into the uterus.
Each procedure has its advantages and disadvantages. IUI is less invasive and less expensive compared to IVF but may have lower success rates in some instances. IVF, on the other hand, offers higher success rates but is more invasive and costly. The choice between the two procedures depends on various factors, including the patient's condition, age, and previous fertility history.
What to Expect During Your GYN Surgery Day
Be prepared and know what to expect on the day of your GYN surgery. You will likely need to arrive at the hospital or surgical center a few hours before the surgery. It is advisable to bring a small bag with any items you may need, such as comfortable clothing, toiletries, and any integral documents or paperwork.
The surgical process involves being prepped for surgery, which includes putting on a hospital gown and having an IV line inserted for fluids and medications. You will receive anesthesia to provide comfort and ensure you're pain-free during the procedure. The time it takes to complete the surgery will vary depending on the procedure.
Post-Operative Care and Recovery Tips
After GYN surgery, proper post-operative care is crucial for a smooth recovery. Your doctor will give you detailed instructions based on your condition and procedure. These instructions may include guidelines for wound care, pain management, activity restrictions, and follow-up appointments.
Follow these instructions diligently to minimize the risk of complications and promote optimal healing. Proper rest, a nutritious diet, staying hydrated, and avoiding strenuous activities are all essential to a successful recovery.
Managing Pain and Discomfort After GYN Surgery
Pain and discomfort are common after GYN surgery, but various options are available to manage them effectively. Your doctor may prescribe pain medications to minimize any post-operative pain. Take these medications as your doctor directs, and do not exceed the recommended dosage.
In addition to medication, applying heat packs or cold compresses to the surgical site can provide relief. Relaxation techniques and gentle stretching can also help manage discomfort. Communicating any persistent or worsening pain to your doctor is essential, as it may indicate a potential complication.
Potential Complications and How to Avoid Them
While GYN surgery is generally safe, potential complications can arise. These may include infection, bleeding, blood clots, damage to surrounding organs, and adverse reactions to anesthesia. However, you can minimize the risk of experiencing these complications by choosing a reputable surgeon, diligently following pre-operative and post-operative instructions, and seeking prompt medical attention if any concerning symptoms arise.
You should be aware of potential complications, such as excessive bleeding, severe pain, fever, or signs of infection. You can ensure a successful outcome by being vigilant and proactive in your recovery.
Frequently Asked Questions About GYN Surgery
- Is GYN surgery painful?
You will receive anesthesia during GYN surgery, so you will not feel any pain. However, you may experience some pain and discomfort after surgery. Your doctor will provide appropriate pain management options to alleviate discomfort. - How long does it take to recover from GYN surgery?
The recovery time after GYN surgery varies depending on the specific procedure and individual factors. It may take a few weeks to recover and resume normal activities fully. Your doctor will provide you with specific guidelines for your recovery period. - Will GYN surgery guarantee successful artificial insemination?
While GYN surgery can significantly improve fertility outcomes for artificial insemination patients, it does not guarantee success. The success of artificial insemination depends on various factors, including the patient's age, overall health, and the quality of sperm or eggs used.
Success Rates and Long-Term Outcomes of Artificial Insemination
The success rates of artificial insemination vary depending on several factors, including the patient's age, the cause of infertility, and the specific procedure performed. On average, the success rates for IUI and ICI range from 10% to 20% per cycle, while IVF and ICSI success rates can be as high as 20% to 35% per cycle.
Long-term outcomes for patients undergoing GYN surgery and artificial insemination are generally positive. By addressing underlying conditions that may hinder conception, GYN surgery increases the chances of successful pregnancy through artificial insemination. However, it is essential to note that individual results may vary, and it is advisable to consult with your doctor for more information regarding your specific case.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
In assisted reproductive technology, Preimplantation Genetic Testing (PGT) has emerged as a crucial tool in the in vitro fertilization (IVF) treatment. PGT testing allows for the screening and diagnosis of genetic abnormalities in embryos before they are transferred to the uterus, increasing the pregnancy success rates and minimizing the risk of genetic disorders. This article will dive into the details of PGT testing, exploring its history, benefits, different types available, accuracy and reliability, role in reducing the risk of genetic disorders, impact on IVF success rates, cost and insurance coverage, ethical considerations, future developments, and frequently asked questions.
Key Takeaways
- PGT testing is a genetic screening tool used in IVF treatment to identify congenital abnormalities in embryos before implantation.
- Different types of PGT testing are available, including PGT-A, PGT-M, and PGT-SR, each with its specific purpose.
- PGT testing can reduce the risk of genetic disorders in offspring and improve IVF success rates.
- The accuracy and reliability of PGT testing have improved over time, making it a valuable tool in IVF treatment.
- While PGT testing can be costly and raises ethical considerations, it will likely continue to play a significant role in the future of IVF treatment.
What is PGT Testing and How Does it Work?
Preimplantation Genetic Testing (PGT) is a laboratory technique used to analyze the genetic makeup of embryos created through IVF treatment. It involves extracting a few cells from an embryo at the blastocyst stage, typically around five to seven days after fertilization. These cells are then analyzed for any genetic abnormalities or chromosomal disorders.
The process of PGT testing begins with embryo biopsy and removing a small sample of cells from the embryo. This sample undergoes various genetic analysis techniques such as polymerase chain reaction (PCR), fluorescence in situ hybridization (FISH), comparative genomic hybridization (CGH), or next-generation sequencing (NGS). These techniques allow for detecting specific genetic abnormalities or chromosomal disorders in the embryo. Once the analysis is complete, the embryos are graded based on their genetic health, and only those deemed to have a higher chance of successful implantation and development are chosen for transfer to the uterus.
The History of PGT Testing in IVF Treatment
The history of PGT testing in IVF treatment dates back to the early 1990s when scientists first began exploring the possibility of screening embryos for genetic abnormalities. The initial focus was on identifying chromosomal disorders such as Down syndrome, which results from an extra copy of chromosome 21. Over the years, technological advancements and an understanding of genetics have led to developing more sophisticated PGT testing methods.
One of the significant milestones in developing PGT testing was the introduction of FISH in the late 1990s. FISH detects specific chromosomal abnormalities by using fluorescent probes that bind to particular DNA sequences. This technique revolutionized PGT testing by enabling the screening of embryos for a range of genetic disorders.
Another milestone in PGT testing came with the advent of CGH in the early 2000s. CGH allowed for a comprehensive analysis of all 23 pairs of chromosomes, providing a more accurate assessment of genetic health. This technique paved the way for more precise embryo selection and improved IVF success rates.

The Benefits of PGT Testing for IVF Patients
| Benefit | Description |
| Increased Pregnancy Rates | PGT testing can identify embryos with chromosomal abnormalities, leading to higher pregnancy rates and lower miscarriage rates. |
| Reduced Risk of Genetic Disorders | PGT testing can identify embryos with genetic disorders, allowing for the selection of healthy embryos and reducing the risk of passing genetic disorders to offspring. |
| Reduced Need for Multiple Embryo Transfers | PGT testing can identify the most viable embryos, reducing the need for multiple embryo transfers and the associated risks and costs. |
| Improved Patient Satisfaction | PGT testing can provide peace of mind for patients, knowing that they have selected the healthiest embryos for transfer. |
PGT testing offers numerous benefits to couples undergoing IVF treatment. Firstly, it significantly improves the chances of a successful pregnancy. By selecting embryos with a higher likelihood of implantation and normal development, PGT testing increases the probability of achieving a healthy pregnancy and live birth.
Secondly, PGT testing reduces the risk of genetic disorders in offspring. By identifying embryos with chromosomal abnormalities or specific genetic mutations, couples can make informed decisions about which embryos to transfer, minimizing the chances of passing on genetic disorders to their children.
Lastly, PGT testing provides couples with increased confidence in embryo selection. By having access to detailed information about the genetic health of their embryos, couples and individuals can decide which embryos to transfer, reducing anxiety and uncertainty during the IVF process.
The Different Types of PGT Testing Available
Several types of PGT testing are available, each with its specific purpose and methodology. Preimplantation Genetic Screening (PGS) is used to screen embryos for chromosomal abnormalities, such as aneuploidy (an abnormal number of chromosomes). PGS is particularly beneficial for couples or individuals with a history of recurrent miscarriages or at a higher maternal age, as these factors increase the likelihood of chromosomal abnormalities in embryos.
On the other hand, Preimplantation Genetic Diagnosis (PGD) is used to diagnose specific genetic disorders in embryos. PGD is best for couples with genetic mutations or a family history of a particular genetic disorder. By identifying embryos affected by the disorder, couples and individuals can make informed embryo selections, reducing the risk of passing on their genetic disorders to their children.
Comparative Genomic Hybridization (CGH) is a technique used in PGT testing to analyze the entire genome of an embryo. CGH provides a comprehensive assessment of all 23 pairs of chromosomes, allowing for the detection of both numerical and structural chromosomal abnormalities. This technique has significantly improved the accuracy and reliability of PGT testing.
Next-generation sequencing (NGS) is a cutting-edge technology revolutionizing PGT testing. NGS allows for the rapid and cost-effective analysis of multiple genes simultaneously, making it an ideal tool for comprehensive genetic screening and diagnosis. NGS has further enhanced the accuracy and efficiency of PGT testing, enabling more precise embryo selection.
The Accuracy and Reliability of PGT Testing
The accuracy and reliability of PGT testing are crucial factors in its success as a diagnostic tool in IVF treatment. The accuracy of PGT testing is typically measured by its ability to identify embryos with or without genetic abnormalities correctly. Studies have shown that PGT testing has a high level of accuracy, with reported rates ranging from 95% to 99%.
The reliability of PGT testing depends on several factors, including the biopsy's quality, the genetic analysis technique's accuracy, and the laboratory's expertise in performing the testing. Couples must choose a reputable and experienced laboratory for PGT testing to ensure reliable results.
While PGT testing is highly accurate, it could be more foolproof. Any diagnostic test, including PGT testing, has a small margin of error. Additionally, PGT testing cannot detect all genetic abnormalities or guarantee a successful pregnancy. However, it significantly improves the chances of a successful pregnancy and does reduce the risk of genetic disorders.
The Role of PGT Testing in Reducing the Risk of Genetic Disorders
One of the primary benefits of PGT testing is its ability to reduce the risk of genetic disorders in offspring. By identifying embryos affected by specific genetic mutations or chromosomal abnormalities, couples can make informed decisions about which embryos to transfer, minimizing the chances of passing genetic disorders to their children.
PGT testing can detect genetic disorders, including single-gene disorders such as cystic fibrosis, sickle cell anemia, and Huntington's disease. It can also identify chromosomal abnormalities such as Down, Turner, and Klinefelter. By identifying embryos affected by these disorders, couples can choose embryos free from genetic abnormalities, significantly reducing the risk of having a child with a genetic disorder.
The Impact of PGT Testing on IVF Success Rates
PGT testing has significantly impacted IVF success rates. By selecting embryos with a higher likelihood of implantation and normal development, PGT testing increases the chances of having a successful pregnancy and live birth.
Studies have shown that PGT testing can improve IVF success rates by up to 30%. This improvement is due to the ability to select genetically healthy embryos with a higher potential for implantation and development. Transferring only the most viable embryos enhances IVF success rates.
Furthermore, PGT testing reduces the risk of implanting embryos with chromosomal abnormalities, which are less likely to result in a successful pregnancy. By screening embryos for aneuploidy and other chromosomal abnormalities, PGT testing ensures that only genetically healthy embryos transfer to the uterus, further improving IVF success rates.
The Cost of PGT Testing and Insurance Coverage
The cost of PGT testing can vary depending on many factors, including the type of testing performed, the number of embryos tested, and the laboratory conducting the testing. On average, PGT testing can cost anywhere from $3,000 to $6,000 per cycle.
Insurance companies may only sometimes cover PGT testing. While some insurance plans may provide coverage for PGT testing, others may consider it an elective procedure and not cover the costs.
Frequently Asked Questions About PGT Testing in IVF
- Is PGT testing necessary for all couples undergoing IVF?
PGT testing is not necessary for all couples undergoing IVF. It is typically best for couples with a history of genetic disorders or chromosomal abnormalities, advanced maternal age, or recurrent miscarriages. - Does PGT testing guarantee a successful pregnancy?
While PGT testing significantly improves the chances of a successful pregnancy, it does not guarantee a successful outcome. Several factors, including the quality of the embryos, the age of the woman, and other individual characteristics, can influence the success of IVF treatment. - Can PGT testing determine the gender of embryos?
Yes, PGT testing can determine the gender of embryos. However, it is essential to note that gender selection for non-medical reasons is considered controversial and may not be available in all countries or clinics. - How long does it take to get the results of PGT testing?
The time it takes to receive the results of PGT testing can vary depending on the laboratory and the specific testing method used. In general, results are typically available within one to two weeks.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is CMV?
CMV, cytomegalovirus, is a member of the herpesvirus family and is highly prevalent worldwide. You can become infected with CMV through bodily fluids, including saliva, urine, blood, seminal fluid, and breast milk. The most common transmission modes are through close contact with infected individuals or exposure to bodily fluids. It is important to note that CMV can be present in an individual's body without causing any symptoms or illness, making detecting and preventing transmission challenging.

How Common is CMV?
The CDC states that nearly 1 in 3 children have already been infected with CMV by age 5, and by the age of 40, over half of the population is infected. The prevalence of CMV in sperm donors varies depending on the screened population. Studies have shown that CMV infection rates among sperm donors range from 30% to 70%. However, it is essential to note that the presence of CMV does not necessarily indicate active infection or the potential for transmission. Donor screening protocols typically include testing for CMV antibodies, which can help determine if the donor has contacted the virus in the past.
Symptoms of CMV Infection
CMV infection can manifest differently in individuals depending on their immune system and overall health. Many people infected with CMV may not experience symptoms or only have mild symptoms that resolve independently. However, those with weakened immune systems, such as individuals with HIV/AIDS or undergoing organ transplantation, may develop severe complications. These can include pneumonia, hepatitis, retinitis (inflammation of the retina), and neurological disorders. Awareness of these symptoms and seeking medical attention if necessary is crucial.
Becoming Infected With CMV
Primary CMV infection occurs in people who have never been exposed to the CMV virus before. Once a person becomes infected with CMV, the virus remains alive but dormant inside their body for the rest of their life. Recurrent CMV infection is when a dormant virus becomes active again. CMV infection is usually harmless and rarely causes illness. However, primary CMV infection can cause more severe problems for pregnant women than recurrent CMV infection.
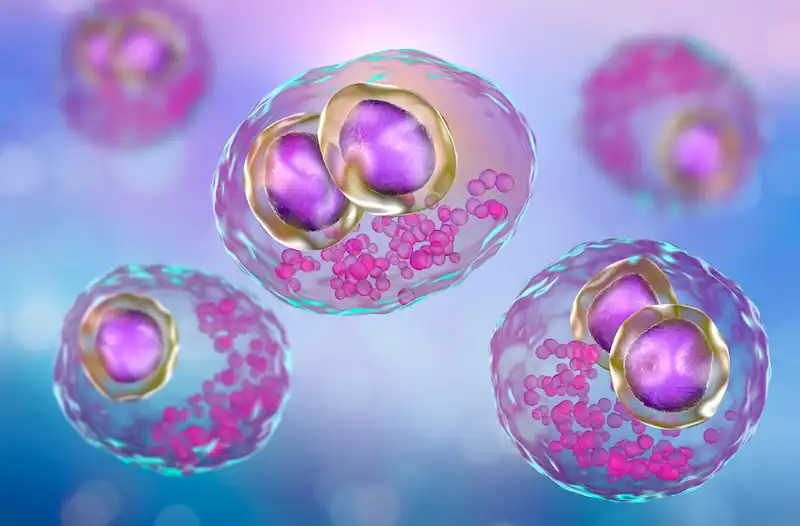
Cytomegalovirus
CMV in human cells.
Diagnosis and Treatment of CMV Infection
Diagnosing CMV infection involves various methods, including blood tests to detect the presence of CMV antibodies or viral DNA. Other tests like urine or saliva samples may also confirm active infection. Treatment options for CMV infection depend on the severity of symptoms and the individual's immune status. A healthcare provider may prescribe antiviral medications to manage the condition and reduce the risk of complications.
Prevention of CMV Transmission in Sperm Donation
Preventing CMV transmission in sperm donation involves following proper protocols and procedures. Donor screening for CMV antibodies is essential in identifying potential donors who may pose a higher risk of transmission. Additionally, implementing strict guidelines for handling and processing donated sperm can help minimize the risk of contamination. Cryopreservation techniques, such as freezing and quarantine periods, can also be employed to ensure that donated sperm is free from infectious agents before use.
CMV Protocols At Cryobank America
The FDA requires CMV testing on all men who intend to donate sperm. A positive result, however, doesn't necessarily mean that a man will be ineligible to donate. Cryobank America will obtain semen samples from potential donors and then quarantine those specimens for at least six months. During that time, the donor may have had CMV antibody levels tested several times. If the antibody tests indicate the possibility of a CMV infection close to the time of the sperm donation, the donor will not be allowed to donate their specimens. If the testing demonstrates inconclusive results, the donor will not be permitted to donate. However, if a donor tests positive for CMV IgG only, indicating a past infection, he will be eligible to contribute. These samples appear in the Cryobank America donor database as CMV-positive.
Can Washed Donor Sperm Transmit CMV?
No, clinically washed sperm is typically free from CMV (Cytomegalovirus) transmission. The sperm-washing process separates sperm from the seminal fluid, which reduces the risk of transmitting infections such as CMV. However, no medical procedure can guarantee 100% elimination of all viruses or infections. You should always consult a healthcare professional for personalized advice and information.
Considering Pregnancy Through Donor Sperm?
Women considering pregnancy with donor sperm should have CMV antibody testing as part of their IDT. Those with a past infection are at low risk of transmitting CMV infection to a fetus and are at little to no risk if they decide to use a CMV-positive donor.
Women never exposed to CMV should consider using a CMV-negative donor. Even though the risk from a CMV-positive donor is low, it is impossible to determine whether there will be a risk for infection.
Cryobank America's donor catalog has a CMV search filter for positive and negative sperm donors. To find a CMV-negative sperm donor, select negative under the CMV option!
CMV Resources
For additional information on CMV, this link is especially helpful:
https://www.mayoclinic.org/diseases-conditions/cmv/symptoms-causes/syc-20355358
If you have any questions about CMV, please email us at [email protected] or call 817-945-8708; we will be happy to help!
One fascinating aspect of artificial insemination is its potential to result in twins. Twins occur when two embryos implant in the uterus and develop simultaneously. Having twins can happen naturally, but artificial insemination can also increase the likelihood of twins due to the controlled introduction of sperm and the manipulation of the woman's reproductive system.
Key Takeaways
- The likelihood of having twins with artificial insemination is higher than natural conception.
- Age significantly affects the chances of having twins with artificial insemination.
- Fertility treatments increase the odds of having twins, with some treatments having higher rates than others.
- Multiple births with artificial insemination could come with risks and complications.
- Preparing for and coping with a twin pregnancy requires planning and management, but resources and support are available.
What are the Chances of Having Twins with Artificial Insemination?
When it comes to the chances of having twins with artificial insemination, statistics show that the likelihood is higher compared to natural conception. According to research, the rate of twin pregnancies with artificial insemination is around 10-30%, depending on various factors such as age and fertility treatments used.
In comparison, the natural occurrence of twins in the general population is approximately 1-2%. This significant difference in rates highlights how artificial insemination can significantly increase the chances of having twins for couples who desire multiple pregnancies.
Factors that Affect the Likelihood of Having Twins with Artificial Insemination
Several factors can influence the likelihood of having twins with artificial insemination. One crucial factor is age. As women age, their chances of naturally conceiving twins decrease. However, with artificial insemination, older women may still have an elevated chance of having twins due to the controlled introduction of sperm and fertility treatments.
Genetics and fertility treatments also increase the odds of conceiving multiples. Some individuals may have a genetic predisposition to releasing multiple eggs during ovulation, increasing their chances of conceiving twins. Additionally, specific fertility treatments, such as in vitro fertilization (IVF), can involve the transfer of multiple embryos, further increasing the likelihood of twins.
Age and Twin Pregnancy: How Age Affects the Chances of Having Twins
| Age Range | Chances of Having Twins | Factors That Increase Chances |
| Under 20 | 1.5% | Family history of twins |
| 20-24 | 1.8% | Family history of twins, taking fertility drugs |
| 25-29 | 2% | Family history of twins, taking fertility drugs |
| 30-34 | 1.9% | Family history of twins, taking fertility drugs |
| 35-39 | 2.3% | Family history of twins, taking fertility drugs, having had multiple pregnancies |
| 40 and Over | 3.5% | Family history of twins, taking fertility drugs, having had multiple pregnancies |
Age significantly contributes to the likelihood of having twins with artificial insemination. Women in their 30s and 40s have higher odds of conceiving twins compared to younger women. This statistic is because older women tend to have more elevated follicle-stimulating hormone (FSH) levels, which can stimulate the ovaries, prompting them to release multiple eggs during ovulation.
However, it's important to note that advanced maternal age also comes with increased risks and complications during pregnancy. Women considering artificial insemination should consult with their healthcare providers, fertility specialists, or OBG-YN to understand the potential risks associated with twin pregnancies at different ages.

Fertility Treatments and Twin Pregnancy: How Fertility Treatments Increase the Chances of Having Twins
Fertility treatments can greatly increase the chances of having twins with artificial insemination. These treatments aim to stimulate the ovaries to produce multiple eggs, increasing the likelihood of fertilization and implantation.
One standard fertility treatment that can result in twins is in vitro fertilization (IVF). During IVF, many embryos are created in a laboratory setting and then transferred into the woman's uterus. Transferring multiple embryos provides a better chance of at least one implanting successfully, potentially resulting in a twin pregnancy.
Types of Fertility Treatments and Twin Pregnancy: Which Treatments are More Likely to Result in Twins?
Different types of fertility treatments have varying rates of success when it comes to achieving a twin pregnancy. In addition to IVF, another commonly used fertility treatment is intrauterine insemination (IUI). During IUI, semen is inserted directly into the woman's uterus, increasing the chances of fertilization.
While IUI has a lower overall success rate compared to IVF, it still has the potential to result in twins. The likelihood of twins with IUI depends on factors such as the woman's age, the number of eggs she releases during ovulation, and the quality of the sperm used.
Multiple Births and Artificial Insemination: Risks and Complications
Although the idea of conceiving twins via artificial insemination may seem thrilling, it is crucial to acknowledge the potential hazards and complexities that come with multiple births. Twin pregnancies are classified as high-risk pregnancies due to the added pressure on the mother's physical well-being and the likelihood of complications.
Twin pregnancies come with a set of potential risks, such as premature births, low birth weight, gestational diabetes, preeclampsia, and placental abnormalities. Therefore, it is of utmost importance for women carrying twins to receive consistent prenatal care and monitoring to gain assurance of the health and well-being of both the mother and babies.
Preparing for a Twin Pregnancy: What to Expect and How to Plan
Preparing for a twin pregnancy requires careful consideration and planning. Expectant parents should educate themselves about the unique challenges of carrying twins and adjust their lifestyle and home environment.
A critical aspect of preparation is ensuring adequate prenatal care. Regular check-ups with healthcare providers will help monitor the status of the pregnancy and address any potential complications early on. Additionally, expectant parents may need to modify their living space, such as purchasing double strollers, cribs, and other essential items for two babies.
Coping with a Twin Pregnancy: Tips for Managing the Challenges
Managing the challenges of a twin pregnancy can be physically and emotionally demanding. Expectant mothers may experience increased fatigue, discomfort, and hormonal changes compared to singleton pregnancies.
Establishing a support network can provide invaluable assistance during this time. Joining twin support groups or online forums designed for parents of multiples can offer a sense of community through shared experiences and advice. Additionally, welcoming professional counseling or therapy can help expectant parents navigate the emotional challenges that may arise during a twin pregnancy.

Understanding the Odds and Making Informed Decisions
Artificial insemination offers couples the opportunity to conceive and experience the joy of parenthood. While the chances of having twins with artificial insemination are higher compared to natural conception, it's essential to consider individual factors such as age, genetics, and fertility treatments when assessing the likelihood of multiple pregnancies.
By understanding the science behind artificial insemination and the factors that influence twin pregnancies, couples can make informed decisions about their reproductive journey. Consulting with healthcare providers, seeking support from resources, and prioritizing self-care are all crucial steps in navigating the challenges and joys of a twin pregnancy.
Resources for Further Information and Support
Various resources are available for further information and support regarding artificial insemination, twin pregnancies, and parenting multiples. Support groups like the Twins Trust and online forums like Twins Magazine provide valuable information, advice, and a platform for connecting with other parents of multiples.
Additionally, healthcare providers specializing in fertility treatments can offer personalized guidance and support throughout the journey. It's important for couples considering artificial insemination or currently carrying twins to access these resources to gain knowledge, find support, and make informed decisions based on their unique circumstances. If you have any questions regarding your chances of having twins with artificial insemination, don't hesitate to contact Cryobank America.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Choosing IUI, ICSI, or At-Home Insemination Over IVF: 4 Factors You Should Know
Exploring different fertility treatment options requires a deep understanding of various factors, ranging from medical to financial, to personal preferences. While In-Vitro Fertilization (IVF) is undoubtedly one of the most recognized fertility treatments, other methods like Intrauterine Insemination (IUI), Intracytoplasmic Sperm Injection (ICSI), and at-home insemination have their unique appeal and benefits. But what drives the decision to choose one over the other? Here, we delve into the reasons.
1. Choosing IVF For Fertility Health and Specific Challenges
The first and foremost consideration is the specific fertility challenge a couple or individual is facing. While IVF is robust and addresses a wide array of fertility issues, some challenges may be addressed more directly with other treatments.
Male Infertility Issues
ICSI, a specialized form of IVF, has emerged as a game-changer for couples dealing with male infertility. By directly injecting a single healthy sperm into an egg, it bypasses challenges like low sperm count or poor sperm mobility. Thus, for those who have identified male infertility as the primary obstacle, ICSI might be a more direct solution than traditional IVF.
Uncomplicated Infertility Or Use Of Donor Sperm
For women with open fallopian tubes, regular ovulation, and no apparent severe infertility issues, IUI provides a less invasive approach. It's particularly popular among single women or lesbian couples using donor sperm.
2. Choosing IUI Or At-Home Insemination Due To Financial Considerations
Fertility treatments can be expensive, and not everyone has the luxury of unlimited resources or comprehensive insurance coverage.
Which Procedure Is Less Expensive, IUI or IVF?
Generally, IUI is less expensive than IVF or ICSI. For those who are on a tighter budget, starting with IUI might be a feasible first step. If several IUI cycles don't result in pregnancy, they might then consider investing in IVF or ICSI.
Cumulative Costs — What's Really More Expensive, IUI or IVF?
It's also essential to consider cumulative costs. While IUI per cycle might be cheaper, if multiple cycles are needed, the costs can add up. In contrast, IVF, though pricier upfront, might offer a higher success rate per cycle. The bottom line will be determined by your overall fertility health, donor or partner compatibility, and timing insemination correctly by precisely tracking your ovulation cycle.
Many cryobanks offer financial services such as payment plans and financing. Cryobank America has partnered with Future Family to offer patients affordable financing options.

3. Choosing IUI, IVF, or At-Home Insemination For Personal Preferences and Comfort
Medical procedures, even if they're routine from a clinical perspective, are deeply personal experiences.
Invasiveness and Comfort — IUI
IUI stands distinct with its simplicity. By directly introducing sperm into the uterus, it bypasses many of the steps intrinsic to IVF, such as egg retrieval and external fertilization. This straightforwardness can be less daunting for those who are apprehensive about medical procedures. The very nature of IUI, being less invasive, can also mean reduced physical discomfort, fewer side effects, and a shorter recovery period.
For many, starting with IUI is a gentle introduction to fertility treatments. The rationale often revolves around giving the less invasive method a try first, hoping it might lead to successful conception without the need for more complex procedures.
Natural Conception
Fertility treatments, for all their medical advancements, can sometimes feel clinical and detached from the intimate experience of conception. This feeling can be a significant determinant in the choices couples make. There's an inherent appeal in procedures that mimic or come close to the process of natural conception.
IUI, especially when executed without the aid of fertility drugs, offers an experience that's remarkably close to natural conception. The process aligns with the body's natural ovulation cycle, and the sperm is introduced directly into the uterus without any external fertilization. This method provides couples with a sense of familiarity and naturalness, making the journey feel less 'medical' and more intimate.
At-Home Insemination
The appeal of at-home insemination lies in its intimacy and privacy. For those who find clinical settings stressful or impersonal, at-home insemination offers a more comfortable and familiar environment. This method is also more cost-effective than clinical procedures, though it may have a lower success rate and lacks the oversight and expertise of a medical setting.
4. Treatment Duration and Timelines
For some, the time it takes from starting treatment to achieving pregnancy is a significant factor.
Which Procedure Is Quicker, IUI or IVF?
IUI stands out as a relatively quicker procedure when juxtaposed against IVF (in vitro fertilization). The simplicity of IUI, which involves directly introducing sperm into the uterus, eliminates several steps intrinsic to the IVF process, such as egg retrieval and lab fertilization. For those already navigating the emotionally charged waters of fertility challenges, the shorter treatment duration of IUI can be a breath of fresh air. It offers hope without the extended commitment, making it an attractive choice for those wary of prolonged medical interventions.
Does IUI or IVF Have A Higher Success Rate?
Time considerations in fertility treatments aren't just about the procedure's speed. It's also about effectiveness across multiple cycles. Here's where the dynamics become intricate. IVF, despite its lengthier process, often touts a higher success rate per cycle when compared to IUI. This statistic can translate to fewer overall treatment cycles, potentially shortening the entire duration from the start of treatment to conception.
On the flip side, the non-invasiveness, simplicity, and lower immediate costs of IUI can lead some to opt for multiple IUI cycles before considering the switch to IVF. The thought process here hinges on hope: the hope that the next IUI cycle might be a successful one, coupled with the procedure's relative simplicity.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Comparing IVF, ICSI, and IUI: Understanding Your Options in Fertility Treatments
Embarking on the path to parenthood, many couples and individuals find themselves at the crossroads of fertility treatments. The journey, while filled with hope, often presents a maze of medical terms, techniques, and decisions. The options — IVF, ICSI, and IUI — though different, all aim to assist in the realization of the dream of having a child. Delving deeper into each method helps demystify the process and sheds light on the complications involved.
Please make sure to also contact a suitable health professional. While this article is your information guide, it is not to be used as a substitute for medical opinion or healthcare treatment.
IVF (In-Vitro Fertilization)
IVF involves stimulating the ovaries using fertility drugs to produce mature eggs. These eggs are then retrieved and fertilized in a lab with sperm from a partner or a donor. The resultant embryo is monitored for signs of fertilization, and the best-quality embryo is transferred to the uterus.
Advantages of IVF
IVF is a comprehensive treatment that can address both male and female infertility factors. Through IVF, mature eggs are retrieved and fertilized in a laboratory setting, and the best-quality embryos are chosen for transfer, increasing the chances of success. The process allows for advanced embryo selection techniques, such as time-lapse monitoring and Preimplantation Genetic Screening. This ensures only embryos with the highest potential are selected. IVF provides the flexibility to use either a partner's or a donor's sperm, giving diverse options for family planning. Additionally, if more than one high-quality embryo results from the cycle, the extra embryos can be frozen for future use.
When is IVF advised?
IVF is typically recommended for those with fallopian tube damage, blockages, or in cases of unexplained infertility. It's also a viable option in mild cases of male infertility.
ICSI (Intracytoplasmic Sperm Injection)
ICSI (Intracytoplasmic Sperm Injection), on the other hand, is a refined version of IVF. Instead of allowing sperm to fertilize the egg naturally in a dish, ICSI involves the direct injection of a single, chosen sperm into the egg. This technique proves invaluable, especially in cases where male infertility is a concern. By bypassing many natural challenges, ICSI offers a chance even when sperm count is low or mobility is compromised.

Advantages of ICSI
ICSI is a specialized form of IVF where a single, healthy sperm is injected directly into the egg. This direct approach maximizes the chance of fertilization, especially in cases of male infertility. Since only the best quality sperm is selected and used, it ensures the highest potential for successful fertilization. ICSI is particularly beneficial when there are significant sperm problems, such as a low sperm count, poor sperm mobility, or high levels of DNA damage in the sperm. Even when sperm needs to be surgically retrieved, ICSI can still be applied. By addressing male fertility issues directly, ICSI bypasses many obstacles that can prevent natural fertilization.
When is ICSI advised?
ICSI is commonly prescribed for those with male fertility problems such as low sperm count, poor sperm mobility, or high levels of DNA damage in sperm. If male fertility isn't the primary issue, IVF is usually the suggested method.
IUI (Intrauterine Insemination)
IUI (Intrauterine Insemination) stands apart from the aforementioned methods. It is less invasive and mirrors the process of natural conception more closely. In this procedure, prepared sperm is directly introduced into the uterus, timed with ovulation, to facilitate fertilization. For many, IUI serves as a starting point in their fertility journey, especially when the primary concern is not related to sperm quality or quantity.
Advantages of IUI
IUI is a straightforward, non-invasive procedure without the need for anesthesia. It's generally more affordable than advanced fertility treatments such as IVF or ICSI. The entire IUI process can be completed within minutes, making it a quick and hassle-free option. The sperm "washing" process ensures that only the best and healthiest sperm are used for insemination. The timing of the insemination is carefully synchronized with the woman's ovulation to increase the chances of success. IUI can effectively address a range of infertility issues, from unexplained infertility to mild male factor problems. It's also a preferred method when using donor sperm, offering a simpler path for diverse family planning. Unlike some other treatments, there's no need for egg retrieval or surgical intervention, making it less physically demanding.
When is IUI advised?
IUI is an option for patients requiring donor sperm. To succeed, it requires clear fallopian tubes, a healthy sperm count, and a mature egg. In cases of irregular ovulation, fertility drugs may be combined with IUI.
Which Treatment is Right for You?
Your unique fertility situation will determine the best treatment. A comprehensive assessment considering your medical history, age, and response to previous treatments is necessary. For some, IUI might be the first step. However, if significant sperm disorders are detected, IVF or ICSI might be more suitable.
It's essential to understand that your fertility journey is individual. The goal is to achieve pregnancy in the most efficient and effective manner. Always ensure that you are part of the decision-making process, aware of the costs, and fully informed about the treatment path ahead.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is ICSI and How Does it Work?
ICSI, or intracytoplasmic sperm injection, is a fertility treatment that involves the direct injection of a single sperm into an egg. This procedure is performed with in vitro fertilization (IVF). During IVF, eggs are retrieved from the woman's ovaries and fertilized with sperm in a laboratory dish. With ICSI, a single sperm is selected and injected directly into each egg, bypassing any potential barriers to fertilization.
The ICSI procedure begins with collecting eggs from the woman's ovaries. These eggs are then placed in a culture dish and examined under a microscope. A single sperm is selected and immobilized using a tiny needle. The needle injects the sperm directly into the egg. After the injection, monitoring the eggs ensures that fertilization occurs. Once fertilization is confirmed, the resulting embryos transfer to the woman's uterus.
Compared to other fertility treatments, such as IVF alone, ICSI offers a higher chance of successful fertilization. This procedure is particularly beneficial for couples who have struggled with male factor infertility, where the quality or quantity of sperm may be compromised due to various factors. ICSI can be helpful in cases where previous attempts at IVF have failed or when there are concerns about the ability of the sperm to penetrate the egg.
Who is a Candidate for ICSI?
Several factors may lead to the need for ICSI.
Male factor infertility is one of the most common reasons for considering ICSI. These factors include low sperm count, poor sperm motility, or abnormal sperm morphology. ICSI can also benefit couples who have experienced previous failed attempts at IVF or have had difficulty achieving fertilization with conventional IVF methods.
Medical Conditions and ICSI
In addition to male factor infertility, certain medical conditions may affect a couple's candidacy for ICSI. These include genetic disorders that are likely to get passed on to offspring, such as cystic fibrosis or Huntington's disease. ICSI can be used with preimplantation genetic testing to screen embryos for these conditions before being transferred to the uterus.
Age Requirements For ICSI
Age can also play a role in determining whether a couple is a good candidate for ICSI. As women age, their ovarian reserve decreases, making achieving successful fertilization and pregnancy more difficult. ICSI can help overcome some of these challenges by directly injecting sperm into the egg, increasing the chances of fertilization.
Preparing for ICSI: What to Expect
Before undergoing ICSI, couples typically have an initial consultation with a fertility specialist. During this consultation, the couple's fertility specialist will review their medical history and discuss any potential factors that may affect the success of ICSI. The fertility specialist may also order additional tests and evaluations to assess the couple's health and fertility potential.
Testing and Evaluations
Medical tests and evaluations may include blood tests to check hormone levels, ultrasounds to evaluate the woman's ovarian reserve and uterine health, and semen analysis to assess the quality and quantity of sperm. These tests will help the fertility specialist determine the most appropriate treatment plan for the couple.
Medications and Injections
In preparation for ICSI, the woman may be prescribed medications to stimulate her ovaries and promote the development of multiple eggs. These medications are generally administered through injections, and the fertility clinic will closely monitor progress and any side effects. The fertility specialist will also advise the woman to make specific lifestyle changes, such as quitting smoking, reducing alcohol consumption, and maintaining a healthy diet and exercise routine.

The ICSI Procedure: Step-by-Step
The ICSI procedure typically follows a specific timeline of events. First, the woman will undergo ovarian stimulation using medications to promote the development of multiple eggs. This step is essential to increase the chances of successful fertilization and pregnancy. During this time, the woman will be closely monitored through ultrasounds and blood tests to assess the growth and maturity of the eggs.
Once the eggs have reached the desired size and maturity, retrieval occurs through a minor surgical procedure called egg retrieval. This procedure is performed under sedation or anesthesia and involves the insertion of a needle into the ovaries to collect the eggs. The eggs are then placed in a culture dish and examined under a microscope.
Next, an embryologist selects a single sperm for each egg. The embryologist carefully examines the sperm under a microscope and chooses the healthiest and most viable sperm for injection. The selected sperm is immobilized using a tiny needle and injected directly into the egg.
After the injection, the eggs are monitored to ensure that fertilization occurs. The presence of two pronuclei confirms successful fertilization. The fertilized eggs, now called embryos, are cultured in the laboratory for a few days before being transferred to the woman's uterus.
Success Rates of ICSI: What to Expect
The success rates of ICSI can vary depending on several factors, including the age of the woman, the quality of the eggs and sperm, and the overall health of the couple. Generally, the success rates of ICSI are comparable to those of conventional IVF, but ICSI can improve your success rate.
Factors that may affect the success rates of ICSI include the woman's age and ovarian reserve. As women age, their ovarian reserve decreases, making achieving successful fertilization and pregnancy more difficult. However, ICSI can help overcome some of these challenges by directly injecting sperm into the egg, increasing the chances of fertilization.
A fertility specialist should discuss realistic expectations during the initial consultation. The fertility specialist can provide personalized guidance based on the individual or couple's circumstances and help manage expectations throughout treatment.
It is also important to note that success rates can vary between fertility clinics. When choosing a fertility clinic for ICSI, it is essential to consider the clinic's success rates and the qualifications and experience of the medical team. A qualified and experienced team can significantly increase the chances of a successful outcome.
After the Procedure: What to Expect
After the ICSI procedure, the woman will typically have a recovery period of a few days. During this time, she may experience discomfort or bloating as her body adjusts to the hormonal changes. A doctor can prescribe pain medication to help manage any discomfort.
A fertility specialist will schedule follow-up appointments to monitor the woman's progress and assess the procedure's success. These appointments may include ultrasounds and blood tests to check for pregnancy and monitor embryo development.
Emotional and psychological considerations are also necessary after the ICSI procedure. Infertility can affect an individual or couple's mental health, and it is crucial to seek support and counseling if needed. Many fertility clinics offer counseling services or can provide referrals to mental health professionals who specialize in infertility.
Alternative Fertility Treatments to Consider
While ICSI is a highly effective fertility treatment, it may not be the right option for every couple. There are several alternative treatments that couples struggling with infertility may consider.
One alternative treatment is intrauterine insemination (IUI), which involves placing sperm directly into the woman's uterus during ovulation. IUI can be a less invasive and less expensive option for couples with mild male factor infertility or unexplained infertility.
In some cases, a fertility specialist may suggest gestational surrogacy. Gestational surrogacy involves using a surrogate to carry the pregnancy for the couple or individual. This process can be an option for couples where the woman cannot carry a pregnancy due to medical reasons.
It is essential for couples and individuals to thoroughly discuss their options with a fertility specialist to determine the most appropriate treatment plan for their specific circumstances.
Choosing the Right Fertility Clinic for ICSI
Choosing the right fertility clinic for ICSI is crucial for a successful outcome. There are several factors to consider when making this decision.
First and foremost, choosing a fertility clinic with a qualified and experienced team is essential. The fertility specialists should have extensive ICSI experience and be board-certified in reproductive endocrinology and infertility.
The success rates of the fertility clinic should also be considered. The clinic should have a track record of high success rates, particularly in cases similar to the couple's specific circumstances.
The clinic's facilities and laboratory should also be state-of-the-art and equipped with the latest technology and equipment. These elements will ensure that the ICSI procedure is performed under optimal conditions.
During the initial consultation with the fertility clinic, asking questions and gathering as much information as possible is essential. This information can include questions about the clinic's success rates, the qualifications and experience of the medical team, and the specific steps and timeline of the ICSI procedure.
Choosing the right fertility clinic can significantly increase the chances of a successful outcome and provide couples with the support and guidance they need during this challenging time.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What Is IUI?
IUI (intrauterine insemination), also known as artificial insemination, is a fertility treatment that involves placing sperm directly into a woman's uterus during her fertile window. This procedure benefits individuals and couples with sperm quality or quantity deficiencies, unexplained infertility, or cervical factor infertility. Unlike IVF, which involves fertilizing the egg outside the body, IUI allows natural fertilization within the woman's body.
A good candidate for IUI is a woman with open fallopian tubes, a normal uterine cavity, a partner with sufficient sperm count and motility, or donor sperm. Couples and individuals must undergo thorough fertility testing and evaluation before proceeding with IUI to ensure it is the appropriate treatment option for their situation.
Preparing for Your First IUI Procedure
Before undergoing an IUI procedure, individuals and couples will typically consult a fertility specialist. During the first consultation, the specialist will perform a physical examination, review your medical history, and discuss any previous fertility treatments or pregnancies. The specialist may also recommend additional fertility testing to determine the cause of infertility and to assess the woman's ovarian reserve.
In preparation for an IUI procedure, lifestyle changes may be recommended by your fertility clinic to improve the chances of success. These changes may include maintaining a healthy weight, avoiding alcohol, and managing stress. Additionally, the woman may be prescribed fertility medications to stimulate the ovaries and increase the number of mature eggs available for fertilization.
What Happens During the IUI Procedure?
The IUI procedure typically occurs in the fertility clinic and does not require anesthesia. The woman will lie on an examination similar to a pelvic exam. The fertility specialist will insert a speculum into the vagina to visualize the cervix. The sperm sample, washed and concentrated to remove impurities, is inserted into the uterus using a thin catheter.
The entire procedure usually takes only a few minutes and is relatively painless. Some women may experience mild cramping or discomfort during the process, but this typically subsides quickly. After the procedure, the woman will lie down briefly to allow the sperm to swim towards the fallopian tubes.

The Role of Fertility Medications in IUI
Fertility medications are often used in conjunction with IUI to increase the chances of success. These medications stimulate the ovaries and promote the development of multiple mature eggs. The most commonly used medications in IUI are oral medications such as Clomid or letrozole, which help regulate ovulation.
In some cases, your fertility clinic may use injectable medications such as gonadotropins to stimulate the ovaries. These medications contain follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which help promote the growth and maturation of multiple eggs. In cases where oral medications have not been successful or more mature eggs are needed, your fertility specialist will use injectable medications.
While fertility medications can increase the chances of success in an IUI procedure, they come with potential side effects. These side effects may include bloating, mood swings, hot flashes, and breast tenderness. Couples must discuss their fertility medications' potential risks and benefits with their fertility specialist before starting treatment.
Potential Risks and Side Effects of IUI
Like any medical procedure, IUI carries some risks. One of the most common risks associated with IUI is the possibility of multiple pregnancies. Because fertility medications stimulate the ovaries and increase the number of mature eggs, there is a higher chance of conceiving twins or even triplets. This risk can be minimized by ensuring your fertility specialist closely monitors your response to fertility medications and adjusts the dosage if necessary.
Regarding side effects, IUI is generally a well-tolerated procedure with minimal discomfort. Some women may experience mild cramping or spotting after the procedure, but these symptoms usually subside within a day or two. Infection or damage to the uterus or fallopian tubes may occur in rare cases, but these complications are extremely rare.
Post-IUI Care and Recovery
After an IUI procedure, couples will typically receive aftercare instructions from their fertility specialist. These instructions may include recommendations for rest, avoiding strenuous activities or exercise, and refraining from sexual intercourse for a certain period. Couples need to follow these instructions to optimize their chances of success.
Most women can resume their normal daily activities after an IUI procedure. However, it is essential to listen to your body and to take it easy if you are experiencing any discomfort or pain. You should also schedule a follow-up appointment with your fertility specialist to discuss your results and determine the next steps.
Interpreting the Results of Your IUI Procedure
The results of an IUI procedure are determined through a pregnancy test, usually done about two weeks after the procedure. A positive result indicates that pregnancy has occurred, while a negative result means pregnancy has not been achieved. It is important to note that a negative result does not necessarily mean the procedure was unsuccessful, as it may take multiple attempts before achieving a successful pregnancy.
If the results of the IUI procedure are positive, it is important to schedule an appointment with an obstetrician or midwife to confirm the pregnancy and to begin prenatal care. You should consult your fertility specialist to discuss the next steps if the results are negative. These may include repeating the IUI procedure, exploring other fertility treatment options such as ICSI or IVF, or further testing to determine the cause of infertility.
What to Do If Your First IUI is Unsuccessful
If your first IUI procedure is unsuccessful, it is important to remember that you are not alone. Many couples require multiple attempts before achieving a successful pregnancy. It is important to discuss the reasons for the unsuccessful IUI with your fertility specialist and to explore other options.
Depending on the circumstances, your fertility specialist may recommend repeating the IUI procedure with or without additional fertility medications. Alternatively, they may suggest exploring other fertility treatment options, such as IVF or intracytoplasmic sperm injection (ICSI). An open and honest discussion with your fertility specialist is crucial to determining the best course of action for your situation.
Exploring Other Fertility Treatment Options
While IUI is a widely used and effective fertility treatment, it may not be the best option for every individual or couple. There are several other fertility treatment options available, including IVF and ICSI.
IVF involves fertilizing the egg outside the body and transferring the resulting embryo(s) into the uterus. ICSI is a similar procedure but involves injecting a single sperm directly into the egg.
When considering other fertility treatment options, you must consider factors such as age, overall health, and the cause of infertility. Consulting with a fertility specialist can help determine the best course of action based on individual circumstances.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States

