Known donor conception refers to the process of using a sperm donor who is known to the intended parents. The donor can be a friend, family member, or someone the intended parents have chosen to be involved in their child's life. The use of a known donor offers several benefits compared to using an anonymous donor:
- It allows for a deeper connection and potential ongoing relationship between the child and the donor.
- It provides the child with the opportunity to have access to valuable medical and genetic information.
- It can be more affordable compared to using donor sperm through a sperm bank.
While using a known donor has its advantages, it is crucial to involve a reputable sperm bank in the process. Sperm banks play a vital role in known donor conception by ensuring the safety and legality of the procedure. They provide a secure environment for donors to undergo medical and psychological evaluations and screening for infectious diseases.
Understanding Sperm Banks and Their Role in Known Donor Conception
A sperm bank is a facility that collects, stores, and distributes sperm samples for use in assisted reproductive procedures such as known donor conception. Sperm banks operate under strict regulations and guidelines to ensure the safety and quality of their services. They are crucial in facilitating known donor conception by providing access to comprehensive screening processes and legal support.
Sperm banks work by recruiting potential donors who undergo thorough medical and psychological evaluations. These evaluations assess the donor's overall health, genetic history, and mental well-being. Donors are also screened for a roster of infectious diseases such as HIV, hepatitis B and C, syphilis, and others. Once a donor passes all necessary screenings, their sperm is collected, processed, and stored in cryogenic tanks at the sperm bank's facility.
To minimize the risk of passing on sexually transmissible infectious through semen specimens, Cryobank America adheres to FDA-mandated requirements, which include the testing and screening of the following:
- ABO blood typing and Rh (Rhesus factor)
- Chlamydia
- Complete Blood Count (CBC)
- Cytomegalovirus (CMV) total antibodies
- Cytomegalovirus (CMV) IgG and IgM antibodies (if total Ab test is positive)
- Gonorrhea
- HIV-1/2/0 Antibodies
- HIV/HCV/HBV NAT
- Hepatitis B surface antigen
- Hepatitis B virus core antibodies
- Hepatitis C virus antibodies
- Human T-cell lymphotropic virus (HTLV-I/II) antibodies
- Syphilis serology
- West Nile Virus NAT
Known donors must undergo a screening process, including a color vision test, a medical social questionnaire (MSQ) form, and a urinalysis. They must also schedule an appointment with our medical director for a thorough physical examination. As an added precaution, we highly recommend that donors opt for genetic screening to identify potential inherited diseases that could affect their offspring.
Choosing a Sperm Bank For Known Donor Conception: Factors to Consider
When choosing a sperm bank for known donor conception, you should consider several factors. Firstly, location and accessibility play crucial roles. Choose a sperm bank that is easily accessible for both the intended parents and the donor. An accessible site ensures convenience throughout the process, especially when coordinating appointments and transporting the donor's sperm.
Reputation and success rates are also important factors to consider. Researching a sperm bank's reputation can provide insight into its track record and customer satisfaction, and success rates can be a big indicator of the quality of its services.
Another crucial factor to consider is the donor selection process. Sperm banks should have a rigorous screening process to ensure their donors' health and suitability. This process includes comprehensive medical evaluations, genetic testing, and psychological assessments. Choose a sperm bank that prioritizes these screenings to minimize potential risks and maximize the chances of a successful conception.
Cost is another significant consideration when choosing a sperm bank. The cost of using a known donor through a sperm bank can vary depending on the services provided. It is essential to inquire about the total cost, including additional storage, shipping, or legal support fees. Cryobank America offers affordable pricing for known donor collections and screenings.

Important Discussions To Have With Your Known Donor
| Discussion Topic | Description |
| Medical history | Discuss any medical conditions, allergies, or genetic disorders that run in the family. |
| Expectations | Discuss each other's expectations regarding involvement in the child's life, financial support, and communication. |
| Legal Considerations | Discuss the legal rights and responsibilities of the donor, the intended parents, and the child. |
| Emotional support | Discuss the emotional support the donor may need during and after the donation process. |
| Future Relationships | Discuss the potential of future relationships between the donor, the intended parents, and the child. |
When embarking on known donor conception, it is crucial to have open and honest discussions with your chosen donor. These discussions should establish expectations and boundaries for all parties involved. Clear communication is critical to ensuring a smooth and respectful process.
One of the most important topics to discuss is the legal considerations and agreements surrounding known donor conception. It is smart to consult with legal professionals specializing in reproductive law to draft a comprehensive agreement outlining the rights and responsibilities of all parties involved. This agreement should address parental rights, financial obligations, and future involvement in the child's life.
Health and genetic testing are also vital to discuss with your known donor. It is essential to ensure that the donor undergoes thorough medical evaluations and genetic testing to reduce the risk of passing on hereditary diseases or conditions. Openly discussing these test results can help make informed decisions about the suitability of the donor.
Additionally, it is crucial to discuss the emotional and psychological aspects of known donor conception. The intended parents and the donor may experience various emotions throughout the process. Discussing these potential challenges and supporting one another can help navigate any difficulties.
The Screening Process for Known Donors
The screening process for known donors at a sperm bank involves several steps to ensure the health and suitability of the donor's sperm. Medical evaluations, including physical examinations, blood tests, and semen analysis, are conducted to assess the overall health of the donor. These evaluations help identify any potential medical issues that could affect fertility or pose risks to future offspring.
Psychological evaluations are also an important part of the screening process. These assessments aim to evaluate the donor's mental well-being and ensure they are emotionally prepared for the responsibilities and potential challenges of known donor conception. These evaluations will cover the donor's motivations, expectations, and understanding of their role in the child's life.
Choosing An Insemination Procedure For Known Donor Sperm
When using known donor sperm, there are several options for insemination procedures to consider. The choice depends on various factors, including the fertility of the intended parent(s), the quality of the donor sperm, and any underlying medical conditions.
Intrauterine insemination (IUI) is a common procedure for known donor conception. It involves placing the prepared sperm directly into the uterus using a catheter. IUI is a fairly simple and non-invasive procedure that can take place in a doctor's office. IUI is a great choice when the intended parent(s) have no significant fertility issues.
Intracervical insemination (ICI) is another option for known donor conception. This procedure involves placing the prepared sperm at the entrance of the cervix, allowing it to swim up into the uterus naturally. Depending on personal preferences and medical advice, ICI can be performed at home or in a clinical setting.
In vitro fertilization (IVF) is a more complex procedure that is best in cases where there are significant fertility issues or when other methods have been unsuccessful. IVF involves fertilizing the eggs with the donor sperm in a laboratory and transferring the fertilized embryos into the uterus. This procedure requires more extensive medical intervention and monitoring.
When choosing an insemination procedure, consider success rates, risks, and personal preferences. Consulting with a fertility specialist can offer valuable guidance in choosing the best option for your circumstances.
Preparing for Insemination: Timing and Fertility Tracking
Timing is crucial in maximizing the chances of successful insemination with known donor sperm. Understanding ovulation and fertility is essential for determining the optimal time to attempt conception.
Ovulation occurs when one ovary releases an egg, which typically occurs once during each menstrual cycle. Various methods can assist in tracking ovulation, including monitoring basal body temperature, tracking changes in cervical mucus, using ovulation predictor kits, or undergoing ultrasound monitoring.
Basal body temperature (BBT) tracking involves measuring your body temperature every morning before you get out of bed. A slight increase in temperature indicates that ovulation has occurred. Tracking changes in cervical mucus consists of observing the consistency and appearance of vaginal discharge. As ovulation approaches, the mucus becomes clearer, stretchier, and more slippery.
Ovulation predictor kits (OPKs) are available over the counter and detect the luteinizing hormone (LH) surge that occurs just before ovulation. These kits are the most accurate choice and can help pinpoint the most fertile days of your cycle. Ultrasound monitoring involves regular visits to a fertility specialist who will use ultrasound technology to monitor the growth and development of follicles in the ovaries.
Timing insemination for optimal chances of success involves having intercourse or performing the chosen insemination procedure within the fertile window, which is typically a few days before and after ovulation. Timing ensures sperm is present in the reproductive tract when the egg is released.
Post-Insemination Care: What to Expect and How to Maximize Your Chances of Success
After insemination with known donor sperm, post-insemination care and monitoring are essential to maximize the chances of successful conception. While there are no guarantees, you can take steps to optimize the chances of a positive outcome.
Post-insemination care involves taking care of your physical and emotional well-being. It is essential to follow any instructions provided by your healthcare provider, including recommendations for rest, activity levels, and medication usage. Avoiding excessive stress, maintaining a healthy lifestyle, and engaging in activities that eliminate stress and promote well-being is also advisable.
Monitoring your body's response to insemination is crucial. Various methods can be used, including tracking basal body temperature, observing changes in cervical mucus, or undergoing blood tests to measure hormone levels. These monitoring techniques can provide insight into the success of the insemination and help determine if further interventions or treatments are necessary.
Maximizing your chances of success involves adopting healthy habits and making lifestyle changes that support fertility. These habits include maintaining a balanced diet, exercising regularly, managing stress levels, avoiding smoking and excessive alcohol consumption, and getting enough sleep. It is also important to continue taking prescribed medications or supplements directed by your healthcare provider.
Dealing with emotional and psychological challenges is integral to the post-insemination period. The journey toward conception can be emotionally taxing, and it is important to seek comfort and support from family and loved ones or professional counselors who specialize in fertility issues. Joining support groups or online forums can also offer a sense of belonging and understanding during this time.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is CMV?
CMV, cytomegalovirus, is a member of the herpesvirus family and is highly prevalent worldwide. You can become infected with CMV through bodily fluids, including saliva, urine, blood, seminal fluid, and breast milk. The most common transmission modes are through close contact with infected individuals or exposure to bodily fluids. It is important to note that CMV can be present in an individual's body without causing any symptoms or illness, making detecting and preventing transmission challenging.

How Common is CMV?
The CDC states that nearly 1 in 3 children have already been infected with CMV by age 5, and by the age of 40, over half of the population is infected. The prevalence of CMV in sperm donors varies depending on the screened population. Studies have shown that CMV infection rates among sperm donors range from 30% to 70%. However, it is essential to note that the presence of CMV does not necessarily indicate active infection or the potential for transmission. Donor screening protocols typically include testing for CMV antibodies, which can help determine if the donor has contacted the virus in the past.
Symptoms of CMV Infection
CMV infection can manifest differently in individuals depending on their immune system and overall health. Many people infected with CMV may not experience symptoms or only have mild symptoms that resolve independently. However, those with weakened immune systems, such as individuals with HIV/AIDS or undergoing organ transplantation, may develop severe complications. These can include pneumonia, hepatitis, retinitis (inflammation of the retina), and neurological disorders. Awareness of these symptoms and seeking medical attention if necessary is crucial.
Becoming Infected With CMV
Primary CMV infection occurs in people who have never been exposed to the CMV virus before. Once a person becomes infected with CMV, the virus remains alive but dormant inside their body for the rest of their life. Recurrent CMV infection is when a dormant virus becomes active again. CMV infection is usually harmless and rarely causes illness. However, primary CMV infection can cause more severe problems for pregnant women than recurrent CMV infection.
Cytomegalovirus
CMV in human cells.
Diagnosis and Treatment of CMV Infection
Diagnosing CMV infection involves various methods, including blood tests to detect the presence of CMV antibodies or viral DNA. Other tests like urine or saliva samples may also confirm active infection. Treatment options for CMV infection depend on the severity of symptoms and the individual's immune status. A healthcare provider may prescribe antiviral medications to manage the condition and reduce the risk of complications.
Prevention of CMV Transmission in Sperm Donation
Preventing CMV transmission in sperm donation involves following proper protocols and procedures. Donor screening for CMV antibodies is essential in identifying potential donors who may pose a higher risk of transmission. Additionally, implementing strict guidelines for handling and processing donated sperm can help minimize the risk of contamination. Cryopreservation techniques, such as freezing and quarantine periods, can also be employed to ensure that donated sperm is free from infectious agents before use.
CMV Protocols At Cryobank America
The FDA requires CMV testing on all men who intend to donate sperm. A positive result, however, doesn't necessarily mean that a man will be ineligible to donate. Cryobank America will obtain semen samples from potential donors and then quarantine those specimens for at least six months. During that time, the donor may have had CMV antibody levels tested several times. If the antibody tests indicate the possibility of a CMV infection close to the time of the sperm donation, the donor will not be allowed to donate their specimens. If the testing demonstrates inconclusive results, the donor will not be permitted to donate. However, if a donor tests positive for CMV IgG only, indicating a past infection, he will be eligible to contribute. These samples appear in the Cryobank America donor database as CMV-positive.
Can Washed Donor Sperm Transmit CMV?
No, clinically washed sperm is typically free from CMV (Cytomegalovirus) transmission. The sperm-washing process separates sperm from the seminal fluid, which reduces the risk of transmitting infections such as CMV. However, no medical procedure can guarantee 100% elimination of all viruses or infections. You should always consult a healthcare professional for personalized advice and information.
Considering Pregnancy Through Donor Sperm?
Women considering pregnancy with donor sperm should have CMV antibody testing as part of their IDT. Those with a past infection are at low risk of transmitting CMV infection to a fetus and are at little to no risk if they decide to use a CMV-positive donor.
Women never exposed to CMV should consider using a CMV-negative donor. Even though the risk from a CMV-positive donor is low, it is impossible to determine whether there will be a risk for infection.
Cryobank America's donor catalog has a CMV search filter for positive and negative sperm donors. To find a CMV-negative sperm donor, select negative under the CMV option!
CMV Resources
For additional information on CMV, this link is especially helpful:
https://www.mayoclinic.org/diseases-conditions/cmv/symptoms-causes/syc-20355358
If you have any questions about CMV, please email us at [email protected] or call 817-945-8708; we will be happy to help!
How To Choose The Right Cryobank — Finding A Donor, Becoming A Donor, And Semen Cryopreservation
Assisted reproduction, whether as a donor or a recipient, involves several crucial decisions. It is a noble endeavor through which one can bring happiness into others’ lives. However, making such a decision requires a thoughtful process. One of the most significant is selecting the right cryobank. A cryobank specializes in the collection, analysis, and storage of human sperm, which can be a lifeline for couples struggling with infertility, single women, or LGBTQ+ couples looking to start a family. Here's a comprehensive guide to navigating the process of choosing the right cryobank, understanding semen cryopreservation, and the intricacies of becoming or finding a donor.
Understanding the Role of a Cryobank
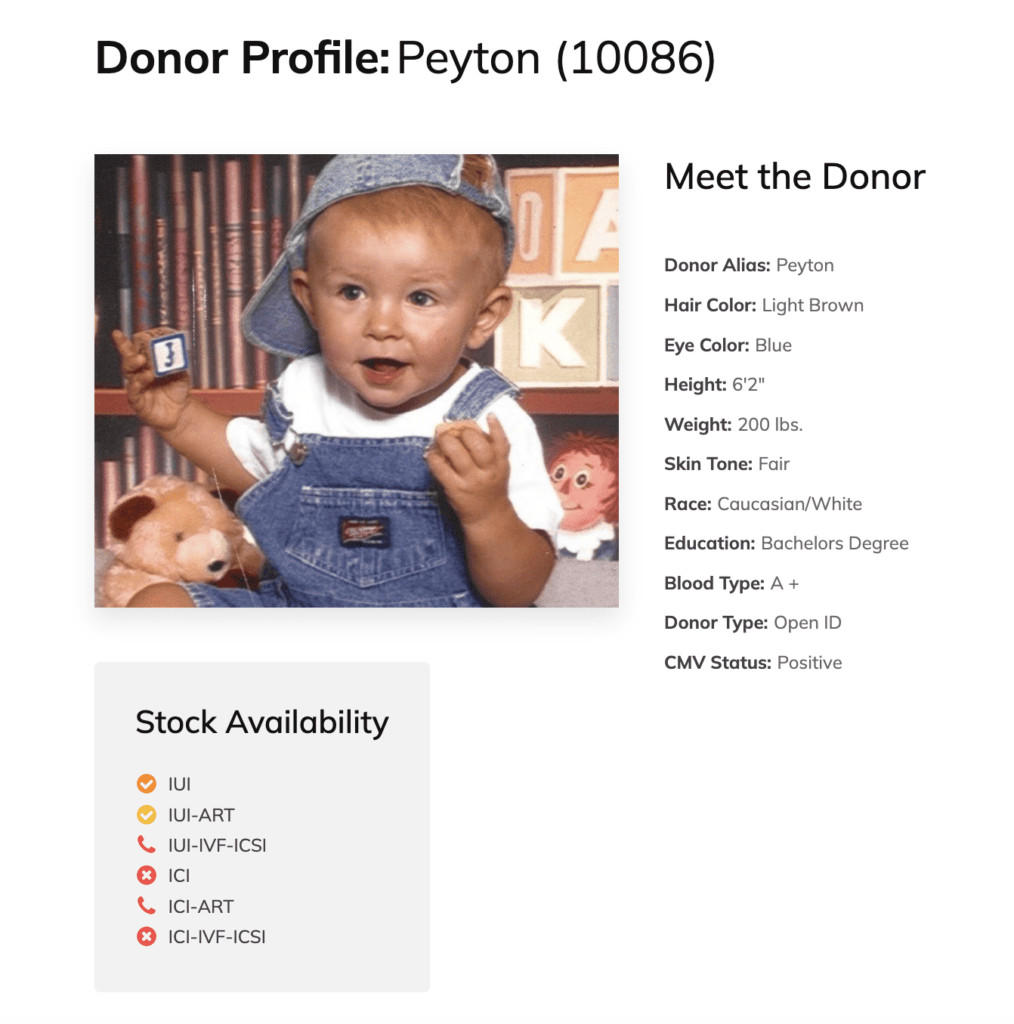
When seeking a sperm donor, several factors come into play. You'll want to consider the donor's health history, physical traits, educational background, and even hobbies or personality traits. Reputable cryobanks provide extensive profiles for each donor, which can help match recipients with donors that meet their specific criteria.
- Diversity and Variety - Look for a cryobank with a wide selection of donors from various ethnic backgrounds, physical characteristics, and personal achievements.
- Transparency - Ensure that the cryobank provides comprehensive medical and psychological screening results of their donors.
- Legal Standards - The cryobank should operate under the strict guidelines set by health authorities and government bodies.
Becoming a Donor: What to Expect
If you're considering becoming a sperm donor, it's important to choose a cryobank with clear, ethical guidelines and rigorous health screening processes.
- Screening Process - Be prepared for in-depth health screenings, including blood tests, semen analysis, genetic testing, and psychological evaluations.
- Commitment - Understand the time commitment involved, as the process might require regular donations for a period.
- Anonymity and Discretion - Decide your preference for future contact with any children born from your donations. Some donors prefer to remain anonymous, while others are open to contact.

Semen Cryopreservation: The Science of Sperm Freezing
Semen cryopreservation, or sperm freezing, is a scientific process where sperm cells are preserved at sub-zero temperatures (-196°C). This process ensures the long-term viability of the sperm, maintaining its integrity for future use in assisted reproductive techniques like In Vitro Fertilization (IVF) or Intrauterine Insemination (IUI). If you are opting for this process, consider the following options.
- Ensure the cryobank uses reliable freezing techniques, guaranteeing the sperm's viability for several years.
- Inquire about the cryobank's procedures for storing and handling the sperm samples to avoid mix-ups or contamination.
- Research the cryobank’s track record with successful pregnancies using their cryopreserved sperm. It's important to note that not all pregnancies are reported to cryobanks, and this statistic may be considerably lower than the true value.
Navigating Costs and Insurance
The services offered by cryobanks, including sperm donation, storage, and assisted reproductive procedures, come with costs. It's important to discuss these details upfront.
- Choose a cryobank that offers clear, upfront pricing for their services.
- Ask if the cryobank accepts health insurance or offers financial plans or assistance.
- Going through assisted reproduction can be emotionally taxing. A good cryobank will provide emotional and logistical support through this journey.
- Look for facilities that offer or recommend professional counseling for donors and recipients.
- Ensure your chosen cryobank has a reliable system for the shipment of sperm samples, especially if you're not located near the facility.
Choosing The Right Cryobank
Choosing the right cryobank is a pivotal decision before embarking on the journey of assisted reproduction, sperm donation, or cryopreservation. Whether you're seeking a sperm donor or are interested in becoming one, it's crucial to select a facility like Cryobank America, which demonstrates a commitment to high ethical standards, comprehensive donor screening, quality cryopreservation methods, and robust support services. Your choice will significantly impact your experience and the success of achieving your dream of starting a family or helping others.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Freezing and Storing Sperm
Sperm freezing is a way for men to save their fertility by freezing and storing their sperm for later use. This technique has become increasingly popular as more individuals recognize the importance of maintaining their reproductive options.
It involves collecting a sperm sample from the individual and subjecting it to a series of steps that prepare it for freezing. A cryobank can store frozen sperm for many years. This storage option allows people to preserve their ability to have children. It benefits those who do not want to start a family immediately.
The history of sperm storage dates back to the 1950s when researchers began experimenting with freezing sperm. Over the years, advancements in technology and techniques have made the process more efficient and successful. Today, sperm storage is a widely accepted method for preserving fertility. Individuals who must undergo cancer treatments or individuals with medical conditions that may affect their fertility also use this method.
The Process of Freezing Sperm
The process of freezing sperm involves several steps to ensure the usability and longevity of the sperm. Once the sample is collected through masturbation, the quality and quantity of the sperm is analyzed.
After the collection and analysis, a cryoprotectant solution is added to the sample. This solution helps protect the sperm from damage during the freezing process. The mixture is divided into small vials or straws labeled and sealed for freezing.
The freezing process typically involves slowly lowering the temperature of the sperm sample to -196 degrees Celsius using liquid nitrogen. This rapid freezing technique is called vitrification.
Vitrification: Rapid Freezing Process
The process of vitrification involves several steps. First, the cells or tissues are treated with a cryoprotectant solution to dehydrate and protect them from freezing damage. Next, they are rapidly cooled to very low temperatures using liquid nitrogen or another cryogenic agent. The rapid cooling prevents the formation of ice crystals and instead forms a glass-like solid.
During vitrification, it is crucial to minimize the exposure of cells or tissues to toxic levels of cryoprotectants. A stepwise approach, where the concentration of cryoprotectants is gradually increased before vitrification, can avoid these harmful levels.
Vitrified samples stored at ultra-low temperatures remain without significant degradation. They can be rapidly thawed and rehydrated for transplantation or research purposes.
Various applications utilize vitrification. Some of these applications include the storage of embryos for in vitro fertilization (IVF), cord blood stem cells, and biological samples for research.
Benefits of Sperm Storage
Sperm storage offers several benefits to individuals who wish to preserve their fertility. One of the primary benefits is the ability to maintain reproductive options in the future. By freezing their sperm, individuals can ensure they have viable sperm available when they are ready to start a family.
Another benefit of sperm storage is the convenience and flexibility it provides. Individuals can freeze their sperm anytime, allowing them to plan for their future without the pressure of starting a family immediately. Storing sperm can benefit individuals pursuing education, career advancement, or other personal goals before beginning a family.
Additionally, sperm storage can reduce the risk of genetic abnormalities in offspring. Freezing sperm at a younger age is very beneficial. It allows individuals to preserve their sperm when it is healthier and less likely to have congenital abnormalities. Storing fertility can be vital for individuals with genetic conditions or a family history of genetic disorders.
Who Can Benefit from Sperm Storage?
Sperm storage can benefit many individuals at risk of fertility loss. It's a smart choice for those who wish to preserve their reproductive options. Some of the groups that can benefit from sperm storage include:
- Certain medical conditions, such as testicular cancer, leukemia, or autoimmune diseases, can affect sperm production or quality. By freezing their sperm before treatment, these individuals can preserve their fertility and increase their chances of having biological children.
- Men undergoing cancer treatment: Chemotherapy and radiation therapy can harm sperm production and quality. Sperm storage before cancer treatment can allow men to have biological children after completing their treatment.
- Men in high-risk occupations exposed to hazardous environments or substances may be at risk of fertility loss. By freezing their sperm, these individuals can protect their fertility and have the option to start a family.
- Men with low sperm counts or poor sperm quality may have difficulty conceiving naturally. By freezing their sperm, they can increase their chances of successful fertilization through assisted reproductive techniques.

Longevity of Frozen Sperm
The longevity of frozen sperm depends on several factors. Storage conditions and the quality of the sperm at the time of freezing are two primary factors. Generally, cryobanks can store frozen sperm for many years without significant loss of viability.
The recommended storage duration for frozen sperm varies depending on the country and the specific regulations in place. In some countries, cryobanks can store frozen sperm for up to 10 years. In other countries, cryobanks can store sperm indefinitely.
Studies have shown that using long-term frozen sperm for assisted reproductive techniques can yield successful outcomes. The success rates of using frozen sperm to achieve pregnancy are comparable to those of using fresh sperm. These rates indicate that frozen sperm can remain viable and capable of fertilization even after many years of storage.
Success Rates of Sperm Storage
The success of sperm storage depends on various factors. Sperm quality, the freezing technique used, and the laboratory's performing procedure expertise are a few factors to consider. Overall, the success rates of using frozen sperm for conception are encouraging.
Studies have shown that the survival rate of frozen sperm after thawing is typically high, ranging from 50% to 80%. Once frozen sperm is thawed, a significant portion remains viable and capable of fertilization.
The success rates of using frozen sperm for assisted reproductive techniques, such as IVF or IUI, are also promising. The chances of achieving pregnancy using frozen sperm are comparable to using fresh sperm. Frozen sperm can be just as effective in achieving conception.
Alternatives to Sperm Storage
Alternative sperm storage options are good for individuals who may not be suitable candidates for this procedure. Some of the alternatives to sperm storage include:
- Testicular Tissue Freezing may be an option for Individuals who cannot produce motile sperm. It could also benefit those at risk of losing their fertility due to medical reasons. Testicular tissue freezing involves removing a small piece of testicular tissue and freezing it for future use.
- Donor sperm is an excellent option for anyone experiencing fertility issues or same-sex couples wanting to start a family. Sperm banks have a collection of donors to choose from. The best part is they're all carefully screened and selected based on the sperm bank's standards. Donor sperm is used in home insemination, intrauterine insemination (IUI), intracervical insemination (ICI), intracytoplasmic sperm injection (ICSI), or in-vitro fertilization (IVF) procedures.
- Adoption can be an excellent option for starting a family. Individuals who cannot conceive naturally or prefer not to pursue assisted reproductive techniques can explore this. Adoption allows individuals to provide a loving home to a child in need.
Individuals must discuss their options with a fertility specialist to determine the most suitable method for preserving their fertility.
The Cost of Sperm Storage
The cost of sperm storage can vary depending on several factors. The cryobank's location, services included, and any additional procedures or tests required to determine the final cost. Sperm storage can range from $500 to $1,500, excluding extra storage or future use fees.
Cryobank America stores sperm for a one-time collection fee of $225 and a monthly storage fee of $18.99. You'll pay a one-time withdrawal fee of $399 when you are ready to use your sample.
Most insurance companies don't cover sperm storage. However, some insurance plans may cover individuals with medical conditions that affect their fertility, such as cancer. Cryobank America has partnered with LIVESTRONG Fertility, offering discounted storage services for registered patients.
Frozen Sperm For Future Fertility
Sperm storage is a valuable option for individuals who wish to preserve their fertility for future use. By freezing and storing their sperm, individuals can maintain their reproductive choices and increase their chances of having future biological children. The process of sperm storage is safe and effective, with high success rates for achieving pregnancy using frozen sperm.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is A Cryobank?
A cryobank, also known as a sperm bank, is a facility that collects, processes, stores, and distributes donated sperm for use in assisted reproductive technologies. Cryobanks play a crucial role in reproductive medicine by providing individuals and couples access to donor sperm when natural conception is not possible or advisable. Cryobanks operate under strict guidelines to ensure the safety and quality of the donated sperm.
The process begins with potential donors undergoing a thorough screening to assess their physical health, medical history, and genetic background. Once accepted as donors, they provide semen samples through masturbation or other collection methods. The samples are then processed to separate the sperm from different components of semen, such as seminal fluid. The processed sperm is then frozen and stored in liquid nitrogen tanks at extremely low temperatures to maintain viability.
What Services Are Typically Offered At A Cryobank?
Semen Analysis
Semen analysis is a laboratory test that examines the characteristics of semen, which is the fluid that contains sperm. It is typically one of the first tests conducted when assessing male fertility. During a semen analysis, several parameters are examined, including sperm count, motility (movement), morphology (shape), and volume of semen. These parameters provide valuable insights into the overall health and quality of sperm.
Semen analysis results can guide fertility treatment decisions. A fertility clinic may recommend different treatment options depending on the analysis findings. For example, if the sperm count is low, assisted reproductive techniques such as intrauterine insemination (IUI) or in vitro fertilization (IVF) may be suggested. On the other hand, if sperm motility is poor, intracytoplasmic sperm injection (ICSI) may be recommended.
Advancements in technology are continuously improving the accuracy and efficiency of semen analysis. For example, computer-assisted sperm analysis (CASA) systems provide more precise measurements of sperm parameters. Ongoing research also explores new ways to assess sperm quality, such as DNA fragmentation testing. These advancements hold promise for improving male fertility assessment and treatment options.
Cryobank Donor Sperm
The process of donor sperm banking involves several steps. First, potential donors undergo a thorough screening process to see if they meet the necessary health and genetic criteria. Once approved, donors provide a semen sample through masturbation or other cryobank-approved methods.
The collected sample is then processed in a laboratory to separate the sperm from other components of semen. The sperm is then mixed with a cryoprotectant solution to protect it during freezing. The sample is divided into vials and frozen using liquid nitrogen. The vials are then stored in a cryogenic tank at extremely low temperatures to maintain the viability of the sperm.
Cryobank facilities adhere to stringent quality control measures to ensure the safety and viability of their samples. When selecting a sperm donor, cryobanks provide various services to assist prospective parents in making informed decisions.
A diverse range of individuals and couples utilizes cryobanks. Some common reasons for using donor sperm include male infertility, genetic disorders, single parenthood by choice, same-sex couples, and couples where the male partner has undergone sterilization procedures.
For individuals or couples facing male infertility, cryobanks offer a solution by providing access to donor sperm. Donor sperm allows them to pursue assisted reproductive technologies such as in vitro fertilization (IVF) or intrauterine insemination (IUI) to achieve pregnancy.
In cases where there is a risk of passing on genetic disorders, using donor sperm can help mitigate that risk. Donors are thoroughly screened for genetic conditions, reducing the chances of passing on inherited diseases to future children.
Single individuals or same-sex couples also rely on sperm banks to fulfill their desire to have children. Sperm donation allows them to start or expand their families, regardless of marital status or sexual orientation.
Click here to view Cryobank America's donor qualifications and screening requirements, or click here to begin your donor search.
Chromosome Analysis
Chromosome analysis is a method of studying genetic makeup by examining the structure and number of chromosomes. This analysis can provide valuable insights into an individual's genetic potential and help identify potential genetic disorders. Chromosome analysis uses several techniques, including karyotyping, fluorescence in situ hybridization (FISH), and comparative genomic hybridization (CGH).
Karyotyping involves staining and examining chromosomes under a microscope to determine their structure and number. This technique can help identify missing or extra chromosomes and structural abnormalities such as translocations or deletions. FISH involves using fluorescent probes to label specific genes or regions of chromosomes, allowing for the detection of specific genetic abnormalities. CGH is a technique that compares the DNA from an individual to a reference DNA sample, allowing for the detection of copy number variations or changes in the number of copies of specific genes.
Chromosome analysis has been instrumental in identifying the genetic basis of inherited traits. Researchers have identified genes contributing to traits such as eye color, height, and intelligence by studying the structure and number of chromosomes. For example, the OCA2 gene on chromosome 15 is associated with the production of melanin, which determines eye color. Variations in this gene can result in different eye colors, such as blue or brown.
Similarly, studies have identified multiple genes on different chromosomes that determine height. These genes interact with each other and environmental factors to influence an individual's height. By studying the structure and number of chromosomes, researchers can better understand the complex genetic basis of traits.

The Myriad Foresight Carrier Screening
The Myriad Foresight Carrier Screen is a cutting-edge genetic testing tool that provides comprehensive screening for over 175 genetic disorders. It utilizes advanced technology to analyze an individual's DNA and identify any mutations or variations that may indicate carrier status for a particular ailment. The Myriad Foresight Carrier Screen is highly accurate and reliable, providing individuals with valuable information about their genetic health.
One of the key advantages of the Myriad Foresight Carrier Screen is its comprehensive nature. It screens for genetic disorders, including those more prevalent in specific ethnic populations. This screening ensures that individuals receive a thorough assessment of their carrier status and can make informed decisions about their family planning options.
The Myriad Foresight Carrier Screen can detect carriers for various genetic disorders. Some specific conditions this screening can identify include cystic fibrosis, spinal muscular atrophy, sickle cell disease, and Tay-Sachs disease, among many others. These disorders vary in severity and prevalence, but all have the potential to impact an individual's health or the health of their future children.
By identifying carriers for these disorders, the Myriad Foresight Carrier Screen allows individuals to understand their risk of passing these conditions to their children. This knowledge can be invaluable in making informed decisions about family planning and taking proactive steps to safeguard the health of future generations.
Complete Bloodwork Testing
Complete bloodwork involves analyzing various components of your blood, including red blood cells, white blood cells, and platelets. Each component plays a crucial role in maintaining your overall health, and abnormalities in their levels can indicate underlying health conditions.
Red blood cells are responsible for carrying oxygen to all parts of your body. A complete blood count (CBC) measures the number of red blood cells in your blood. Abnormal levels of red blood cells can indicate anemia, which can be caused by a deficiency in iron, vitamin B12, or folic acid can cause. It can also indicate other underlying health conditions like kidney disease or bone marrow disorders.
White blood cells are essential to your immune system and help fight off infections and diseases. A CBC also measures the number of white blood cells in your blood. Elevated levels of white blood cells can indicate an infection or inflammation in your body. On the other hand, low levels of white blood cells can be a sign of a weakened immune system or certain medical conditions such as leukemia.
Platelets are responsible for clotting your blood to prevent excessive bleeding. A CBC also measures the number of platelets in your blood. Abnormal levels of platelets can indicate a bleeding disorder or a bone marrow disorder.
Cryobank Sperm Storage
Sperm storage is a critical aspect of cryobanks. Sperm can be stored in a cryobank for extended periods, allowing individuals or couples to use the sperm when they are ready to start a family.
The sperm storage process involves freezing the sperm samples in liquid nitrogen at extremely low temperatures. This freezing process helps preserve the viability of the sperm by slowing down cellular activity. Sperm can be stored in liquid nitrogen tanks for many years without significantly losing quality.
Cryobanks offer different storage options depending on individual needs and preferences. Some individuals may choose short-term storage if they plan to use the sperm within a few months or years. Others may opt for long-term storage to preserve their fertility for an extended period, such as cancer patients undergoing chemotherapy or radiation therapy.
The recommended storage duration for sperm varies depending on individual circumstances. Cryobanks can store sperm for several years without significant loss of quality. Still, it is important to consult with a fertility specialist to determine the best storage duration for your specific situation.
Known Donor Collection
Known sperm donor collection offers several benefits for families seeking to conceive through sperm donation. One of the main advantages is the potential for a stronger emotional connection and support system. When using a known sperm donor, there is the opportunity for ongoing communication and involvement between the donor, parents, and child. This involvement can create a sense of extended family and provide additional emotional support for all parties involved.
Additionally, having a known sperm donor can give families a sense of security and peace of mind. They can establish a relationship with the donor before conception, which can help build trust and ensure that the donor is a good fit for their family. Known donors are still required to undergo testing, which includes medical screening, blood testing, semen analysis, urinalysis, and more. They also have the option to receive additional screenings such as genetic testing or chromosome analysis.
Cryobank At-Home Insemination Kit
At-home insemination, also known as self-insemination, is a method used by individuals or couples trying to conceive without the assistance of a medical professional. It involves introducing sperm into the reproductive system to achieve pregnancy. Insertion is performed through various methods, such as using a sterile syringe or a cervical cap.
At-home insemination differs from other fertility treatments, such as in vitro fertilization (IVF) or intrauterine insemination (IUI) because it does not require medical intervention or fertility drugs. It is a more natural and less invasive method that individuals and couples can perform in the comfort of their own homes.
At Cryobank America, the process of at-home insemination is simple. Once you've chosen your perfect sperm donor, you'll place your vial order online. We'll schedule delivery of your vials around your schedule and fertility window. You'll receive our at-home insemination kit with everything you need to complete self-insemination. Click here for an in-depth overview of our process and steps for success.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Our Mission
Cryobank America is committed to providing high-quality reproductive services to individuals and couples looking to start or expand their families. Our mission is to offer a diverse range of sperm donors, ensuring everyone can access the best options for their unique needs.
Why Diversity in Our Donor Collection is Important to Us
Background and Cultural Heritage
We understand the importance of diversity and inclusivity in our donor pool. Regardless of race or ethnicity, every individual should have the opportunity to find a donor who reflects their background and cultural heritage. That's why we are constantly working towards recruiting more ethnically diverse sperm donors.

Representing All Races and Ethnicities
Diversifying the sperm donor pool is crucial for several reasons. Firstly, it ensures that all races and ethnicities have representation and access to donor sperm. By having a diverse collection of donors, individuals or couples seeking a donor can find a match that aligns with their racial or ethnic background, preserving cultural and familial ties.
Genetic Compatibility
Furthermore, diversity in sperm donation is essential for matching donors with recipients. Genetic compatibility plays a significant role in the success of assisted reproduction techniques. By having a diverse donor collection, healthcare providers can better match recipients to donors with similar genetic traits, increasing the chances of a successful pregnancy.
Equal Access
Lastly, diversity in sperm donation promotes social justice and equity. It challenges the notion that certain races or ethnicities are more desirable than others and promotes the idea that everyone deserves equal access to reproductive technologies. By diversifying the sperm donor pool, we can create a more inclusive and equitable society.
How You Can Help Us Expand Our Donor Database
By expanding our donor database to include a broader range of ethnicities, we aim to provide a more comprehensive selection for our clients. We recognize that representation matters, so we do everything possible to create an inclusive environment where everyone feels valued and respected.
If you want to become a sperm donor with Cryobank America, we encourage individuals from all backgrounds to apply. Your contribution can make a significant difference in someone's life and help fulfill their dreams of starting a family. We welcome diversity and value the unique qualities that each individual brings.
Celebrate the Beauty of Diversity
Join us in creating a more diverse and inclusive community by becoming part of Cryobank America. Together, we can help individuals and couples achieve their dreams of parenthood while celebrating the beauty of diversity.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
How To Prepare For At-Home Insemination Before Placing Your Vial Order
At-home insemination is a method of assisted reproduction that allows couples to conceive without medical intervention. It involves using donor sperm to inseminate the female partner at home. You can use any of our vial options for at-home insemination. However, our premium IUI and ICI vials are recommended over all other options, which you can learn more about by clicking here.
One of the main benefits of at-home insemination is the privacy and convenience it offers. Couples can avoid the stress and expense of fertility clinics and have more control over the process. Whether you are purchasing donor sperm for at-home insemination or to have a procedure performed at your fertility clinic, our Clinic Release Form must be signed and submitted to us before you can complete your online purchase.
First Steps in Preparing for At-Home Insemination
Health & Wellness Check
Before placing your vial order with Cryobank America, ensuring both partners are in good health and have undergone necessary medical check-ups and testing is essential. This assurance includes checking for any underlying medical conditions affecting fertility and testing for sexually transmitted infections. It is also advisable to consult with a healthcare professional to ensure that at-home insemination is a safe and appropriate option for you.

Timing is Everything: Effectively Tracking Your Ovulation Before Scheduling Your Vial Delivery
Understanding ovulation and fertility is crucial for maximizing the chances of conception through at-home insemination. You must plan your vial delivery just before your fertility window.
Several methods are available for tracking ovulation, including tracking basal body temperature, monitoring cervical mucus, using ovulation predictor kits, or tracking changes in the cervix. Each method has advantages and considerations, so trying different ways to find the one that works best for you may be helpful.
Timing insemination correctly is crucial for increasing the chances of conception. That's why we don't consider ovulation-tracking mobile apps to be a reliable method. These mobile applications can only provide a vague approximate fertility window. Use ovulation testing kits designed to track ovulation precisely and provide detailed instructions. Typically, these kits will include testing strips that monitor the presence and concentration of luteinizing hormone (LH) in your urine, which appears about 12 – 36 hours before ovulation. Insemination should occur within a day or two before ovulation or on the day of ovulation itself. Perfectly timing insemination ensures that the sperm is present in the reproductive tract when the egg is released, increasing the chances of fertilization.
I Ordered Donor Sperm, and My Vials Are Out for Delivery. What's Next?
Once you've purchased your vials from Cryobank America and our team has coordinated an excellent delivery time based on your schedule, you will receive a USPS tracking code. Your tracking code will tell you the exact date and approximate delivery time.
Once your delivery arrives, you'll receive your vials along with our at-home insemination kit. Our kit includes a pre-charged dry shipper containing your purchased vials, complete documentation, and a sterile syringe.
Our dry shippers are pre-charged in our laboratory to remain active during shipping. They transport biological specimens safely and hold cryogenic temperatures of -150°C or colder. Our dry shippers are manufactured with compounds that absorb liquid nitrogen, ensuring there won't be any spills during shipping. Each dry shipper ships inside a protective container to provide an additional layer of protection.
Your At-Home Insemination Kit
Your delivery will also include four valuable pieces of documentation consisting of the following:
- A package summary. Your summary will list what you ordered, including the vial type, quantity, and total cost for your purchase. It will also include an analysis of your vial's motility and sperm count.
- Infectious Disease Report. This information includes your selected donor's most recent lab testing and infectious/non-infectious disease reports.
- Complete instructions. This paperwork will guide you on handling your dry shipper, thawing your specimen, and performing insertion.
- Package return slip. We will also provide a return slip for your dry shipper.
Lastly, you will receive a ready-for-use sterile syringe. Remember, you have seven days from the shipment date to complete the insertion. If shipping your vials and accompanying equipment takes two days, you will have five days to perform at-home insemination.
Tips for Successful At-Home Insemination
Creating a comfortable and safe environment is very important during insemination. Make sure your space is clean and free from distractions. It may be helpful to create a relaxing atmosphere by playing soothing music or using aromatherapy.
Experts recommend lying flat or with your hips elevated for 25-30 minutes following gentle insertion. You can inseminate once if you're confident in your fertility window calculation. If unsure, consider inseminating twice.
Climaxing through clitoral stimulation can also increase your chances of conception. When a woman climaxes, her cervix becomes more receptive to sperm.
Refrain from strenuous exercise for a few days following insemination and continue to eat healthy. Eliminate processed foods with a high list of ingredients and stick to whole foods as long as possible. Avoid foods that are hard to digest, such as red meats, greasy foods, and refined sugar. Drinking alcohol or using tobacco products isn't recommended during your insemination, as they harm egg quality and fertility.
How We Can Help You Through Your Journey
Our assistance doesn't stop at shipping your vials! If you have any questions before, during, or after you've initiated your insemination, don't hesitate to pick up the phone. We've helped many individuals and couples who have embarked on this journey already, and we look forward to applying our expertise and genuine care to help make everything as easy and stress-free as possible.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is In Vitro Fertilization?
In vitro fertilization (IVF) is a fertility treatment that has helped millions of couples worldwide conceive and start families. It involves a complex process of fertilizing eggs outside the body and transferring them to the uterus. While IVF has become increasingly common, it is vital to understand the science behind it to make informed decisions about fertility treatments.
Understanding the Basics of IVF Fertility Treatments
IVF is a fertility treatment that involves fertilizing eggs outside the body and transferring them to the uterus. It is used when other fertility treatments have failed, or underlying medical conditions make it difficult to conceive naturally. The process involves several steps, including hormone therapy to stimulate egg production, retrieval, fertilization, and embryo transfer.
Not everyone is a candidate for IVF, and it is essential to consult with a fertility specialist to determine if it is the right option for you. Factors such as age, medical history, and overall health can all impact the success of IVF.
The Role of Hormones in IVF Fertility Treatments
There are several types of hormones used in hormone therapy for IVF fertility. These include follicle-stimulating hormone (FSH), luteinizing hormone (LH), human chorionic gonadotropin (hCG), and gonadotropin-releasing hormone (GnRH). FSH and LH are used to stimulate the ovaries to produce multiple eggs. hCG is used to trigger ovulation, which is necessary for egg retrieval. GnRH is used to prevent premature ovulation.
Hormone therapy is typically administered over several weeks leading up to egg retrieval. Your fertility specialist should carefully monitor the timing and dosage of the medications to ensure that the ovaries are responding appropriately and that ovulation occurs at the optimal time for egg retrieval.
The Process of Egg Retrieval in IVF Fertility Treatments
Egg retrieval is a critical step in the IVF process, as it involves removing mature eggs from the ovaries for fertilization. The procedure typically involves using ultrasound guidance to locate the follicles containing mature eggs, then using a needle to extract them.
While egg retrieval is generally safe, it can have risks such as bleeding, infection, and damage to surrounding organs. Timing is also important in egg retrieval, as eggs must be retrieved at the right time to maximize their chances of fertilization.
The Importance of Sperm Quality in IVF Fertility Treatments
Sperm quality is crucial in IVF, as healthy sperm are necessary for successful fertilization. Factors such as age, lifestyle habits, and underlying medical conditions can all impact sperm quality.
Techniques such as intracytoplasmic sperm injection (ICSI) may be used to improve sperm quality and increase the chances of fertilization. ICSI involves injecting a single sperm directly into an egg, bypassing any potential issues with sperm motility or morphology.
The ICSI procedure involves several steps. First, the eggs are retrieved from the woman's ovaries using ultrasound-guided aspiration. The eggs are then placed in a culture dish and prepared for injection.
Next, a single sperm is selected and immobilized using a microneedle. The needle is then used to inject the sperm directly into the egg's cytoplasm. After injection, the eggs are monitored for signs of fertilization.
The Role of Embryo Development in IVF Fertility Treatments
Embryo development is critical to IVF, as healthy embryos are necessary for a successful pregnancy. Following fertilization, the embryo undergoes a series of cell divisions, progressing from two to four cells. By the fifth or sixth day, the embryo reaches the blastocyst stage, marking the optimal time for transfer into the uterus.
Advancements in IVF technology have led to improved patient success rates and outcomes. For example, preimplantation genetic testing (PGT) can help identify congenital abnormalities in embryos before they are transferred into the uterus.
Other possibilities for improving embryo development and implantation include using artificial intelligence (AI) to analyze embryo images and predict which embryos will most likely result in successful pregnancies.
The Emotional and Psychological Impact of IVF Fertility Treatments
IVF can have a significant emotional and psychological impact on patients and their partners. Common challenges include stress, anxiety, and depression. Coping strategies such as therapy or support groups can help manage these challenges.
IVF Fertility Treatments
Research and development in IVF technology continue to advance, with potential innovations such as artificial intelligence and gene editing on the horizon.
IVF fertility treatments have helped millions of couples worldwide conceive and start families. Understanding the science behind IVF is crucial for making informed decisions about fertility treatments.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
The Average Success Rate for Artificial Insemination
Artificial insemination (AI) is a fertility treatment that involves placing sperm directly into a woman's reproductive system to increase the chances of pregnancy. It is a popular option for couples struggling with infertility or for same-sex couples who wish to conceive. The average success rate for artificial insemination ranges between 5% to 30% per cycle, and success can depend on several factors. Understanding these factors is crucial for making informed decisions about your fertility treatments.
Factors Affecting the Success Rate For Artificial Insemination
Several factors can affect the success rate of artificial insemination, including sperm quality, timing, age, and fertility drugs.
What's the most important factor? You guessed it; it's sperm quality! Healthy sperm is necessary for fertilization, and poor sperm quality can significantly reduce the chances of pregnancy. Timing is also crucial, as insemination must occur during the woman's fertile window. Age is another factor affecting success rates, as fertility declines with age. Fertility drugs are often used to stimulate ovulation and increase the chances of pregnancy. Finally, the selected method for artificial insemination can impact the outcome for success.
Understanding the Role of Sperm Quality in the Success Rate For Artificial Insemination
Sperm quality refers to the ability of sperm to fertilize an egg and produce a viable pregnancy. Various factors such as sperm count, motility, morphology, and DNA integrity determine the overall quality. High-quality sperm is essential for achieving successful pregnancies through artificial insemination. Poor sperm quality can lead to low fertility rates, reduced conception rates, and increased risk of embryonic loss.
The impact of poor sperm quality on fertility rates cannot be overstated. Women who inseminate with low-quality sperm can result in failed pregnancies or offspring with genetic abnormalities. Therefore, it is crucial to ensure that you are receiving high-quality sperm for your artificial insemination procedure.
Several factors can affect sperm quality, including environmental and genetic factors. Environmental factors such as temperature, nutrition, and stress can significantly impact sperm quality. High temperatures can damage sperm cells, while poor nutrition can lead to reduced sperm production and motility. Stress can also affect sperm quality by decreasing testosterone levels and increasing oxidative stress.
Genetic factors also play a crucial role in determining sperm quality. That's why we only accept high-quality applicants with desirable traits to improve the overall genetic quality of offspring produced through artificial insemination.
At Cryobank America, we offer premium-grade IUI vials. IUI vials are a great choice because they include sperm that has undergone a density gradient separation wash. This method purifies and isolates the healthiest cells, removing biological debris and seminal fluid, ultimately increasing your success rate. Click here to learn more about our vial types. Click here to view vial pricing.

The Importance of Timing in Artificial Insemination
Timing is crucial in achieving pregnancy through artificial insemination. The window of opportunity for successful insemination is relatively small, and missing it can significantly reduce the chances of conception. Sperm can survive in the female reproductive system for up to five days, but the egg is only viable for 12-24 hours after ovulation. Therefore, it is essential to time the introduction of sperm correctly to coincide with ovulation.
The timing of insemination can also affect the quality of sperm that reaches the egg. Sperm inside of the female reproductive system for too long may become less motile and less capable of fertilizing an egg. On the other hand, introducing sperm too early can result in a lower concentration of sperm, reducing the chances of successful fertilization.
Understanding the menstrual cycle and its phases is crucial to achieving successful insemination. The menstrual cycle is divided into three phases: follicular, ovulatory, and luteal. The follicular phase begins on the first day of menstruation and lasts until ovulation. During this phase, follicles in the ovaries mature and prepare to release an egg.
The ovulatory phase is when ovulation occurs, and an egg is released from the ovary. This phase typically lasts 24 hours but can extend up to 48 hours. Finally, during the luteal phase, the body prepares for pregnancy by thickening the uterine lining.
The timing of insemination is critical during the ovulatory phase since the egg is released from the ovary and travels down the fallopian tube. Therefore, tracking menstrual cycles can help determine when ovulation occurs and increase the chances of successful insemination.
The Impact of Age on the Success Rate For Artificial Insemination
The biological clock refers to the natural decline in fertility that occurs as women age. As women age, their eggs become less viable, and the chances of conceiving naturally or through fertility treatments decrease. This decline in fertility is due to a decrease in the number and quality of eggs available for fertilization.
Age also impacts the success rates of artificial insemination. Studies have shown that women over 35 have lower success rates with artificial insemination than younger women. Older women have fewer viable eggs and are more likely to have underlying fertility issues that can impact the success of the treatment.
Studies have shown that women under 35 have success rates of around 20% per cycle with artificial insemination; however, this success rate decreases as women age. Women over 35 have success rates of approximately 10% per cycle, and women over 40 have success rates of around 5% per cycle. Women are born with a finite number of eggs, and as they age, the number and quality of these eggs decline. When a woman reaches her mid-30s, her fertility begins to fall rapidly.
Other age-related factors impacting success rates include underlying fertility issues, such as endometriosis or polycystic ovary syndrome (PCOS), and lifestyle factors, such as smoking or obesity.
The Role of Fertility Drugs in Artificial Insemination
Fertility drugs are often used in conjunction with artificial insemination to increase the chances of pregnancy. These drugs work by stimulating ovulation and increasing the number of eggs available for fertilization.
Several fertility drugs are available, including Clomifene citrate (Clomid), Metformin, and Gonadotropins. These drugs can significantly increase the chances of pregnancy when used correctly.
Tips for Maximizing the Success of Artificial Insemination
Several lifestyle changes can help maximize the success rate of artificial insemination, including maintaining a healthy weight, reducing stress levels, and avoiding smoking and excessive alcohol consumption.
Choosing the proper fertility treatment and clinic is imperative for the best outcome. Preparing for the procedure by carefully following all instructions can also increase the chances of pregnancy. Finally, post-insemination care is crucial for ensuring a healthy pregnancy.
Advances in AI technology are continually improving success rates and making personalized treatments more accessible than ever. Understanding success rates is crucial for making informed decisions about fertility treatments and achieving a successful pregnancy.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Understanding the Importance of Choosing the Right Sperm Donor
Choosing the right sperm donor is crucial for anyone considering donor insemination. The process of selecting a donor can seem overwhelming, but it is essential to take the time to make an informed decision. Like traditional conception, a sperm donor can significantly impact a child's health, development, and emotional well-being. In this article, we will explore the importance of choosing a suitable sperm donor and help guide you in making the best decision for you and your family.

Health and Genetic Factors to Consider When You Select Your Ideal Sperm Donor
A child's genetic makeup plays a significant role in their health and development. When choosing a sperm donor, one must consider their medical history and genetic health. Genetic conditions can be passed down from a parent to their child, and it is crucial to ensure that the donor does not carry any genetic mutations that could cause health problems for the child. That's why Cryobank America conducts rigorous screenings on all of our donors before their specimens are accepted into our program. These screenings include infectious and non-infectious diseases, a complete blood count, urinalysis, drug testing, and chromosome analysis. Once you've shown interest in a particular donor, we can provide you with their history of health, history of fertility, and family medical history.
In addition to physical health, the emotional and psychological impact of knowing one's biological origins is also essential to consider. Children conceived through donor insemination may have questions about their biological origins, so it is important to understand your donor's psychological traits. As part of joining our Sperm Donor Program, each donor must visit a psychiatrist and undergo a complete mental health evaluation. Cryobank America is one of the few clinics requiring this step to participate in a donor program.
Background and Educational Factors to Look For During Your Donor Search
Throughout your journey of finding a perfect sperm donor, there are factors to consider other than overall health and genetics. These include education, occupation, personal values, and interests.
Education and occupation can tell you a lot about a donor, such as their primary interests, level of intelligence, and how much drive and focus they acquire. Some parents may want a donor with a high education level or a particular occupation, while others may place less emphasis on these factors. Regardless of your preference, Cryobank America verifies this criterion with every donor who enters our program, requiring all potential donors to have a college degree. To ensure the safety of your selection, we also perform a complete criminal history background check on all of our donors.

Physical Characteristics and Traits are Good Things to Consider Before Making Your Sperm Donor Selection
Physical characteristics and traits are also important to consider. Some parents may want a donor with similar physical characteristics, while others may prioritize height, eye color, or hair color.
Personal values and interests can also be essential to consider. Some parents may want a donor who shares their religious or political beliefs, while others prioritize other values and interests.
Cryobank America has an eclectic roster of donors as we aim to provide various physical and personality attributes. Our donors fill out a characteristic questionnaire, write a handwritten letter, and create a donor essay, helping you feel like you've gotten to know them. When you sign up for our Premium Membership, you'll unlock this valuable information, additional childhood photos, and an audio interview!
The Role of Donor Profiles in Sperm Donor Selection
Donor profiles are an essential tool in the sperm donor selection process. Interpreting sperm donor profiles can be challenging, especially regarding medical terminology and genetic testing results. It's important to review each profile carefully and understand the information provided to identify any concerns. Look for donors who meet your criteria regarding medical history, physical characteristics and traits, education and occupation, and personal values and interests. Prioritize your preferences and decide based on what is most important to you and your family.
At Cryobank America, our basic donor profiles include one childhood photo, alias name, donor ID number, height, weight, blood type, hair color, eye color, skin tone, race, the highest level of education, and CMV status. These basic attributes will help guide you in selecting the perfect sperm donor.
Making the Decision to Choose Anonymous vs. Open Sperm Donors
There are legal and ethical considerations to consider when selecting a sperm donor. It is essential to understand the legal rights and responsibilities of sperm donors and recipients and to evaluate the ethical implications of donor anonymity and disclosure.
One of the most significant decisions parents must make when selecting a sperm donor is whether to choose an anonymous or open donor. Anonymous donors do not agree to be contacted by the child in the future, while open sperm donors accept the possibility of contact.
There are benefits and drawbacks to both anonymous and open sperm donors. Anonymous donors provide privacy and anonymity that some parents may prefer. In contrast, open donors allow for the opportunity for the child to learn more about their biological origins.
Select Your Ideal Sperm Donor: Tips and Resources for Success
Finding the ideal sperm donor may seem complicated; that's why we've gathered many resources to help keep you on the right track! Our reputable donor database provides a wealth of information about our donors, and there are many helpful articles and tips available for guidance and support right here on our website.
Choosing the most suitable sperm donor is crucial for anyone considering donor insemination. By taking the time to make an informed decision, you can ensure the best possible outcome for your child's health, development, and emotional well-being.
Click here to get started or click here to learn about our Conception Commitment™ Program!
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States