Polycystic ovary syndrome (PCOS)
PCOS is a hormonal disorder characterized by multiple cysts on the ovaries. The exact cause of PCOS is unknown, but it is believed to be a combination of genetic and environmental factors. Women with PCOS have higher levels of androgens (male hormones) and insulin in their bodies, which can disrupt the normal functioning of the ovaries.
PCOS and its Impact on Fertility
PCOS can have a significant impact on fertility. The hormonal imbalances associated with PCOS can interfere with the regular ovulation process, making it difficult for women to release mature eggs for fertilization. This can result in irregular or absent menstrual periods, making it challenging to predict ovulation and time intercourse for conception. Additionally, cysts on the ovaries can further disrupt the ovulation process.
Common Symptoms of PCOS
Common symptoms of PCOS-related infertility include irregular menstrual cycles, anovulation (lack of ovulation), and difficulty getting pregnant. Women with PCOS may also experience other symptoms, such as weight gain, acne, excessive hair growth, and insulin resistance. It is important for women experiencing these symptoms to seek medical evaluation and diagnosis to determine if PCOS is the underlying cause of their infertility.
Endometriosis
Endometriosis is a chronic condition in which the tissue that lines the uterus, known as the endometrium, grows outside the uterus. This tissue can implant and grow on the ovaries, fallopian tubes, and other organs in the pelvic area. As a result, it can cause inflammation, scarring, and the formation of adhesions, which are bands of fibrous tissue that can bind organs together.

How Endometriosis Can Lead to Infertility
When endometriosis affects the reproductive system, it can lead to infertility. Endometrial tissue outside the uterus can interfere with the normal functioning of the ovaries, fallopian tubes, and uterus. It can cause blockages in the fallopian tubes, preventing the sperm from reaching the egg for fertilization. It can also affect the quality of the eggs produced by the ovaries and interfere with the implantation of a fertilized egg in the uterus.
Symptoms of Endometriosis
Symptoms of endometriosis can vary from woman to woman, but common signs include pelvic pain, painful periods, heavy or irregular bleeding, pain during intercourse, and infertility. It is essential for women experiencing these symptoms to seek medical attention to receive a proper diagnosis and appropriate treatment.
Pelvic inflammatory disease (PID)
PID is an infection that occurs when bacteria from the vagina or cervix travel up into the uterus, fallopian tubes, or ovaries. This infection can happen due to sexually transmitted infections (STIs) such as chlamydia or gonorrhea, but it can also occur due to other types of bacteria. The infection causes inflammation in the pelvic organs, leading to symptoms such as pelvic pain, abnormal vaginal discharge, and fever.
Common Causes of PID
Common causes of PID include unprotected sex with multiple partners, a history of STIs, and the use of intrauterine devices (IUDs). It is critical to seek medical attention if you experience symptoms of PID, as early diagnosis and treatment can help prevent complications such as infertility.
PID and its Impact on Fertility
PID can have a significant impact on fertility in women. The infection can cause scarring and damage to the fallopian tubes, making it difficult for eggs to travel from the ovaries to the uterus. This damage can result in infertility or an increased risk of ectopic pregnancy, where the fertilized egg implants outside the uterus.
In addition to tubal damage, PID can lead to other reproductive complications, such as chronic pelvic pain, ovarian cysts, and adhesions (scar tissue) in the pelvic organs. These issues can further contribute to infertility and make it challenging to conceive.
Statistics show that PID is a leading cause of infertility worldwide. According to the Centers for Disease Control and Prevention (CDC), about 1 in 8 women with a history of PID experience difficulties getting pregnant. Individuals with PID should know these risks and seek appropriate medical care and support.
Uterine fibroids
Uterine fibroids are incredibly common, with studies estimating that up to 70% of women will develop fibroids by age 50. These growths can vary in size and number, and while many women may have fibroids without experiencing symptoms, others may experience heavy menstrual bleeding, pelvic pain, and fertility issues.

How Uterine Fibroids Impact Fertility
Uterine fibroids can impact fertility in several ways. Firstly, the presence of fibroids can alter the shape and size of the uterus, making it difficult for a fertilized egg to implant properly. Fibroids can also block or distort the fallopian tubes, preventing sperm from reaching the egg.
Additionally, fibroids can disrupt the blood supply to the uterus, leading to decreased blood flow to the endometrium (the uterus lining). Decreased blood flow can affect embryo implantation and increase the risk of miscarriage. Furthermore, fibroids can cause uterine inflammation, interfering with the implantation process.
Treatment Options for Uterine Fibroids
Various treatment options are available for uterine fibroids, depending on the size, location, and symptoms associated with the fibroids. These include medication, minimally invasive procedures such as uterine artery embolization or focused ultrasound surgery, and surgical removal of fibroids.
The treatment choice will depend on factors such as the severity of symptoms, desire for future fertility, and overall health. In some cases, treatment of fibroids can improve fertility outcomes by removing obstacles to conception and implantation.
Thyroid disorders
Thyroid disorders and infertility are closely intertwined. Research studies have consistently shown a higher prevalence of thyroid disorders among individuals struggling with infertility than among the general population. For example, a study published in the Journal of Clinical Endocrinology & Metabolism found that women with unexplained infertility were more likely to have thyroid disorders than fertile women.
Another study published in the journal Fertility and Sterility found that women with hypothyroidism (underactive thyroid) had a significantly higher rate of infertility than those without thyroid disorders. Similarly, women with hyperthyroidism (overactive thyroid) also had a higher rate of infertility than those without thyroid disorders.
These studies highlight the importance of recognizing and addressing thyroid disorders in individuals struggling with infertility. Treating the underlying thyroid condition can improve their chances of successful conception and pregnancy.
How Thyroid Disorders Impact Fertility
Thyroid disorders can cause menstrual irregularities, significantly impacting ovulation and conception. When the thyroid gland is not functioning correctly, it can disrupt the normal hormonal balance necessary for regular menstrual cycles.
Irregular periods can make it difficult to predict ovulation, which is crucial for successful conception. Without regular ovulation, it becomes challenging to time intercourse correctly and increase the chances of fertilization.
Treatment Options for Menstrual Irregularities Caused by Thyroid Disorders
Treatment options for menstrual irregularities caused by thyroid disorders depend on the underlying cause of the problem. In some cases, treating the thyroid disorder itself may help regulate menstrual cycles and improve ovulation. In other instances, additional interventions such as hormonal therapy or fertility treatments may be necessary to restore regular menstrual cycles and increase the chances of successful conception.
Diabetes
Diabetes can disrupt the delicate balance of reproductive hormones in both men and women. In women, diabetes can lead to irregular menstrual cycles, anovulation (lack of ovulation), and hormonal imbalances such as high testosterone levels. These hormonal imbalances can make it more difficult for women to conceive and increase the risk of conditions such as polycystic ovary syndrome (PCOS).
Insulin resistance is a common feature of diabetes, particularly in type 2 diabetes. It occurs when the body's cells become less responsive to insulin, leading to elevated blood sugar levels. Insulin resistance can have a significant impact on female fertility.
Diabetes and Conception
Maintaining good blood sugar control is essential for individuals with diabetes trying to conceive. Elevated blood sugar levels can affect the quality of eggs and sperm, making it more difficult for fertilization to occur. High blood sugar levels can also increase the risk of pregnancy complications, such as gestational diabetes and preeclampsia.
By keeping blood sugar levels within a target range, individuals with diabetes can optimize their fertility and improve their chances of a healthy pregnancy. Regular monitoring, following a balanced diet, exercising regularly, and taking medication as prescribed by a healthcare professional can help keep blood sugar levels within a normal range.
Managing Fertility With These Conditions
It is important to note that while these conditions can negatively impact fertility, many can be managed or treated with medical intervention. Consulting with a healthcare professional or fertility specialist is recommended for individuals experiencing difficulties conceiving. With the proper diagnosis and treatment, a fertility specialist can inform you which fertility treatments are best for you.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
How To Prepare For At-Home Insemination Before Placing Your Vial Order
At-home insemination is a method of assisted reproduction that allows couples to conceive without medical intervention. It involves using donor sperm to inseminate the female partner at home. You can use any of our vial options for at-home insemination. However, our premium IUI and ICI vials are recommended over all other options, which you can learn more about by clicking here.
One of the main benefits of at-home insemination is the privacy and convenience it offers. Couples can avoid the stress and expense of fertility clinics and have more control over the process. Whether you are purchasing donor sperm for at-home insemination or to have a procedure performed at your fertility clinic, our Clinic Release Form must be signed and submitted to us before you can complete your online purchase.
First Steps in Preparing for At-Home Insemination
Health & Wellness Check
Before placing your vial order with Cryobank America, ensuring both partners are in good health and have undergone necessary medical check-ups and testing is essential. This assurance includes checking for any underlying medical conditions affecting fertility and testing for sexually transmitted infections. It is also advisable to consult with a healthcare professional to ensure that at-home insemination is a safe and appropriate option for you.

Timing is Everything: Effectively Tracking Your Ovulation Before Scheduling Your Vial Delivery
Understanding ovulation and fertility is crucial for maximizing the chances of conception through at-home insemination. You must plan your vial delivery just before your fertility window.
Several methods are available for tracking ovulation, including tracking basal body temperature, monitoring cervical mucus, using ovulation predictor kits, or tracking changes in the cervix. Each method has advantages and considerations, so trying different ways to find the one that works best for you may be helpful.
Timing insemination correctly is crucial for increasing the chances of conception. That's why we don't consider ovulation-tracking mobile apps to be a reliable method. These mobile applications can only provide a vague approximate fertility window. Use ovulation testing kits designed to track ovulation precisely and provide detailed instructions. Typically, these kits will include testing strips that monitor the presence and concentration of luteinizing hormone (LH) in your urine, which appears about 12 – 36 hours before ovulation. Insemination should occur within a day or two before ovulation or on the day of ovulation itself. Perfectly timing insemination ensures that the sperm is present in the reproductive tract when the egg is released, increasing the chances of fertilization.
I Ordered Donor Sperm, and My Vials Are Out for Delivery. What's Next?
Once you've purchased your vials from Cryobank America and our team has coordinated an excellent delivery time based on your schedule, you will receive a USPS tracking code. Your tracking code will tell you the exact date and approximate delivery time.
Once your delivery arrives, you'll receive your vials along with our at-home insemination kit. Our kit includes a pre-charged dry shipper containing your purchased vials, complete documentation, and a sterile syringe.
Our dry shippers are pre-charged in our laboratory to remain active during shipping. They transport biological specimens safely and hold cryogenic temperatures of -150°C or colder. Our dry shippers are manufactured with compounds that absorb liquid nitrogen, ensuring there won't be any spills during shipping. Each dry shipper ships inside a protective container to provide an additional layer of protection.
Your At-Home Insemination Kit
Your delivery will also include four valuable pieces of documentation consisting of the following:
- A package summary. Your summary will list what you ordered, including the vial type, quantity, and total cost for your purchase. It will also include an analysis of your vial's motility and sperm count.
- Infectious Disease Report. This information includes your selected donor's most recent lab testing and infectious/non-infectious disease reports.
- Complete instructions. This paperwork will guide you on handling your dry shipper, thawing your specimen, and performing insertion.
- Package return slip. We will also provide a return slip for your dry shipper.
Lastly, you will receive a ready-for-use sterile syringe. Remember, you have seven days from the shipment date to complete the insertion. If shipping your vials and accompanying equipment takes two days, you will have five days to perform at-home insemination.
Tips for Successful At-Home Insemination
Creating a comfortable and safe environment is very important during insemination. Make sure your space is clean and free from distractions. It may be helpful to create a relaxing atmosphere by playing soothing music or using aromatherapy.
Experts recommend lying flat or with your hips elevated for 25-30 minutes following gentle insertion. You can inseminate once if you're confident in your fertility window calculation. If unsure, consider inseminating twice.
Climaxing through clitoral stimulation can also increase your chances of conception. When a woman climaxes, her cervix becomes more receptive to sperm.
Refrain from strenuous exercise for a few days following insemination and continue to eat healthy. Eliminate processed foods with a high list of ingredients and stick to whole foods as long as possible. Avoid foods that are hard to digest, such as red meats, greasy foods, and refined sugar. Drinking alcohol or using tobacco products isn't recommended during your insemination, as they harm egg quality and fertility.
How We Can Help You Through Your Journey
Our assistance doesn't stop at shipping your vials! If you have any questions before, during, or after you've initiated your insemination, don't hesitate to pick up the phone. We've helped many individuals and couples who have embarked on this journey already, and we look forward to applying our expertise and genuine care to help make everything as easy and stress-free as possible.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is In Vitro Fertilization?
In vitro fertilization (IVF) is a fertility treatment that has helped millions of couples worldwide conceive and start families. It involves a complex process of fertilizing eggs outside the body and transferring them to the uterus. While IVF has become increasingly common, it is vital to understand the science behind it to make informed decisions about fertility treatments.
Understanding the Basics of IVF Fertility Treatments
IVF is a fertility treatment that involves fertilizing eggs outside the body and transferring them to the uterus. It is used when other fertility treatments have failed, or underlying medical conditions make it difficult to conceive naturally. The process involves several steps, including hormone therapy to stimulate egg production, retrieval, fertilization, and embryo transfer.
Not everyone is a candidate for IVF, and it is essential to consult with a fertility specialist to determine if it is the right option for you. Factors such as age, medical history, and overall health can all impact the success of IVF.
The Role of Hormones in IVF Fertility Treatments
There are several types of hormones used in hormone therapy for IVF fertility. These include follicle-stimulating hormone (FSH), luteinizing hormone (LH), human chorionic gonadotropin (hCG), and gonadotropin-releasing hormone (GnRH). FSH and LH are used to stimulate the ovaries to produce multiple eggs. hCG is used to trigger ovulation, which is necessary for egg retrieval. GnRH is used to prevent premature ovulation.
Hormone therapy is typically administered over several weeks leading up to egg retrieval. Your fertility specialist should carefully monitor the timing and dosage of the medications to ensure that the ovaries are responding appropriately and that ovulation occurs at the optimal time for egg retrieval.
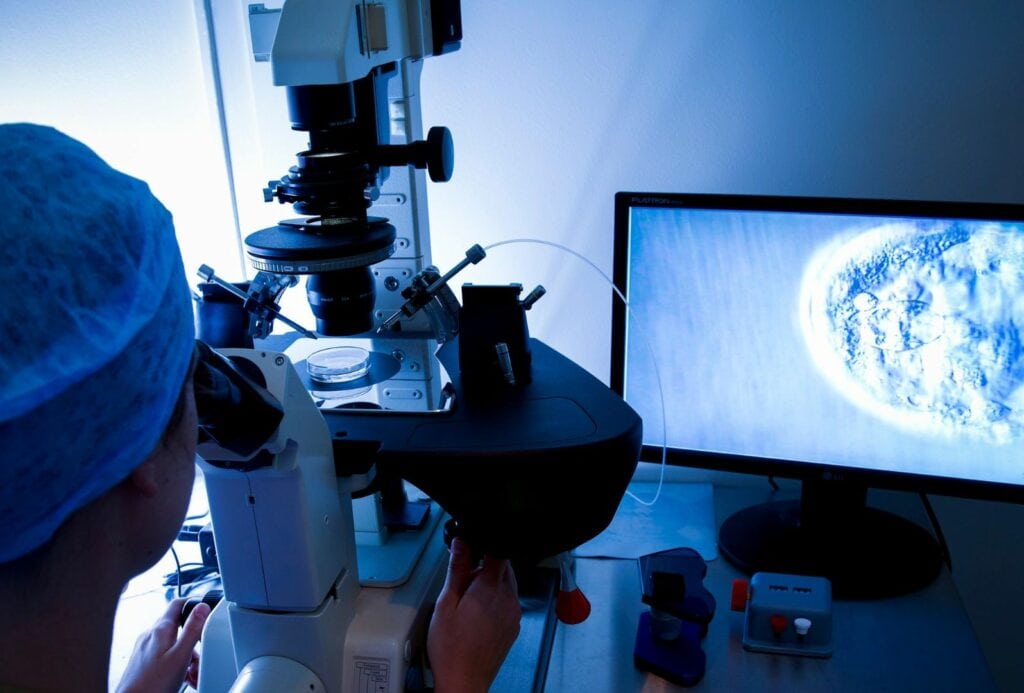
The Process of Egg Retrieval in IVF Fertility Treatments
Egg retrieval is a critical step in the IVF process, as it involves removing mature eggs from the ovaries for fertilization. The procedure typically involves using ultrasound guidance to locate the follicles containing mature eggs, then using a needle to extract them.
While egg retrieval is generally safe, it can have risks such as bleeding, infection, and damage to surrounding organs. Timing is also important in egg retrieval, as eggs must be retrieved at the right time to maximize their chances of fertilization.
The Importance of Sperm Quality in IVF Fertility Treatments
Sperm quality is crucial in IVF, as healthy sperm are necessary for successful fertilization. Factors such as age, lifestyle habits, and underlying medical conditions can all impact sperm quality.
Techniques such as intracytoplasmic sperm injection (ICSI) may be used to improve sperm quality and increase the chances of fertilization. ICSI involves injecting a single sperm directly into an egg, bypassing any potential issues with sperm motility or morphology.
The ICSI procedure involves several steps. First, the eggs are retrieved from the woman's ovaries using ultrasound-guided aspiration. The eggs are then placed in a culture dish and prepared for injection.
Next, a single sperm is selected and immobilized using a microneedle. The needle is then used to inject the sperm directly into the egg's cytoplasm. After injection, the eggs are monitored for signs of fertilization.
The Role of Embryo Development in IVF Fertility Treatments
Embryo development is critical to IVF, as healthy embryos are necessary for a successful pregnancy. Following fertilization, the embryo undergoes a series of cell divisions, progressing from two to four cells. By the fifth or sixth day, the embryo reaches the blastocyst stage, marking the optimal time for transfer into the uterus.
Advancements in IVF technology have led to improved patient success rates and outcomes. For example, preimplantation genetic testing (PGT) can help identify congenital abnormalities in embryos before they are transferred into the uterus.
Other possibilities for improving embryo development and implantation include using artificial intelligence (AI) to analyze embryo images and predict which embryos will most likely result in successful pregnancies.
The Emotional and Psychological Impact of IVF Fertility Treatments
IVF can have a significant emotional and psychological impact on patients and their partners. Common challenges include stress, anxiety, and depression. Coping strategies such as therapy or support groups can help manage these challenges.
IVF Fertility Treatments
Research and development in IVF technology continue to advance, with potential innovations such as artificial intelligence and gene editing on the horizon.
IVF fertility treatments have helped millions of couples worldwide conceive and start families. Understanding the science behind IVF is crucial for making informed decisions about fertility treatments.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
The Average Success Rate for Artificial Insemination
Artificial insemination (AI) is a fertility treatment that involves placing sperm directly into a woman's reproductive system to increase the chances of pregnancy. It is a popular option for couples struggling with infertility or for same-sex couples who wish to conceive. The average success rate for artificial insemination ranges between 5% to 30% per cycle, and success can depend on several factors. Understanding these factors is crucial for making informed decisions about your fertility treatments.
Factors Affecting the Success Rate For Artificial Insemination
Several factors can affect the success rate of artificial insemination, including sperm quality, timing, age, and fertility drugs.
What's the most important factor? You guessed it; it's sperm quality! Healthy sperm is necessary for fertilization, and poor sperm quality can significantly reduce the chances of pregnancy. Timing is also crucial, as insemination must occur during the woman's fertile window. Age is another factor affecting success rates, as fertility declines with age. Fertility drugs are often used to stimulate ovulation and increase the chances of pregnancy. Finally, the selected method for artificial insemination can impact the outcome for success.
Understanding the Role of Sperm Quality in the Success Rate For Artificial Insemination
Sperm quality refers to the ability of sperm to fertilize an egg and produce a viable pregnancy. Various factors such as sperm count, motility, morphology, and DNA integrity determine the overall quality. High-quality sperm is essential for achieving successful pregnancies through artificial insemination. Poor sperm quality can lead to low fertility rates, reduced conception rates, and increased risk of embryonic loss.
The impact of poor sperm quality on fertility rates cannot be overstated. Women who inseminate with low-quality sperm can result in failed pregnancies or offspring with genetic abnormalities. Therefore, it is crucial to ensure that you are receiving high-quality sperm for your artificial insemination procedure.
Several factors can affect sperm quality, including environmental and genetic factors. Environmental factors such as temperature, nutrition, and stress can significantly impact sperm quality. High temperatures can damage sperm cells, while poor nutrition can lead to reduced sperm production and motility. Stress can also affect sperm quality by decreasing testosterone levels and increasing oxidative stress.
Genetic factors also play a crucial role in determining sperm quality. That's why we only accept high-quality applicants with desirable traits to improve the overall genetic quality of offspring produced through artificial insemination.
At Cryobank America, we offer premium-grade IUI vials. IUI vials are a great choice because they include sperm that has undergone a density gradient separation wash. This method purifies and isolates the healthiest cells, removing biological debris and seminal fluid, ultimately increasing your success rate. Click here to learn more about our vial types. Click here to view vial pricing.

The Importance of Timing in Artificial Insemination
Timing is crucial in achieving pregnancy through artificial insemination. The window of opportunity for successful insemination is relatively small, and missing it can significantly reduce the chances of conception. Sperm can survive in the female reproductive system for up to five days, but the egg is only viable for 12-24 hours after ovulation. Therefore, it is essential to time the introduction of sperm correctly to coincide with ovulation.
The timing of insemination can also affect the quality of sperm that reaches the egg. Sperm inside of the female reproductive system for too long may become less motile and less capable of fertilizing an egg. On the other hand, introducing sperm too early can result in a lower concentration of sperm, reducing the chances of successful fertilization.
Understanding the menstrual cycle and its phases is crucial to achieving successful insemination. The menstrual cycle is divided into three phases: follicular, ovulatory, and luteal. The follicular phase begins on the first day of menstruation and lasts until ovulation. During this phase, follicles in the ovaries mature and prepare to release an egg.
The ovulatory phase is when ovulation occurs, and an egg is released from the ovary. This phase typically lasts 24 hours but can extend up to 48 hours. Finally, during the luteal phase, the body prepares for pregnancy by thickening the uterine lining.
The timing of insemination is critical during the ovulatory phase since the egg is released from the ovary and travels down the fallopian tube. Therefore, tracking menstrual cycles can help determine when ovulation occurs and increase the chances of successful insemination.
The Impact of Age on the Success Rate For Artificial Insemination
The biological clock refers to the natural decline in fertility that occurs as women age. As women age, their eggs become less viable, and the chances of conceiving naturally or through fertility treatments decrease. This decline in fertility is due to a decrease in the number and quality of eggs available for fertilization.
Age also impacts the success rates of artificial insemination. Studies have shown that women over 35 have lower success rates with artificial insemination than younger women. Older women have fewer viable eggs and are more likely to have underlying fertility issues that can impact the success of the treatment.
Studies have shown that women under 35 have success rates of around 20% per cycle with artificial insemination; however, this success rate decreases as women age. Women over 35 have success rates of approximately 10% per cycle, and women over 40 have success rates of around 5% per cycle. Women are born with a finite number of eggs, and as they age, the number and quality of these eggs decline. When a woman reaches her mid-30s, her fertility begins to fall rapidly.
Other age-related factors impacting success rates include underlying fertility issues, such as endometriosis or polycystic ovary syndrome (PCOS), and lifestyle factors, such as smoking or obesity.
The Role of Fertility Drugs in Artificial Insemination
Fertility drugs are often used in conjunction with artificial insemination to increase the chances of pregnancy. These drugs work by stimulating ovulation and increasing the number of eggs available for fertilization.
Several fertility drugs are available, including Clomifene citrate (Clomid), Metformin, and Gonadotropins. These drugs can significantly increase the chances of pregnancy when used correctly.
Tips for Maximizing the Success of Artificial Insemination
Several lifestyle changes can help maximize the success rate of artificial insemination, including maintaining a healthy weight, reducing stress levels, and avoiding smoking and excessive alcohol consumption.
Choosing the proper fertility treatment and clinic is imperative for the best outcome. Preparing for the procedure by carefully following all instructions can also increase the chances of pregnancy. Finally, post-insemination care is crucial for ensuring a healthy pregnancy.
Advances in AI technology are continually improving success rates and making personalized treatments more accessible than ever. Understanding success rates is crucial for making informed decisions about fertility treatments and achieving a successful pregnancy.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Consider Yoga Before Donating Sperm
Yoga is a practice that has been around for thousands of years and provides numerous benefits for the mind, body, and soul. In recent years, there has been a growing interest in using yoga to improve male fertility, particularly in the context of sperm donation for at-home insemination. This article will explore the concept of Namaste and Conceive, which is the idea of using yoga to improve sperm quality and quantity for successful insemination.
Understanding the Importance of Sperm Quality Before Donating
Sperm quality plays a crucial role in successful insemination. Poor sperm quality can lead to infertility and can also affect pregnancy outcomes. That's why we won't accept sperm samples that fail to meet our criteria. Sperm count, motility, and morphology determine sperm quality. Low sperm count means that there are fewer sperm available for fertilization, while poor motility means the sperm cannot swim effectively toward the egg. Abnormal morphology refers to the shape and size of the sperm, which can also affect their ability to fertilize the egg.

How Yoga Can Improve Sperm Quality and Quantity
Research has shown that yoga can improve male fertility by improving sperm count, motility, and morphology. Yoga helps reduce stress, a significant factor that can negatively impact male fertility. Stress can affect the production of testosterone, which is essential for sperm production. Yoga also helps to improve blood flow to the reproductive organs, which can increase the production of healthy sperm.
The Role of Stress in Fertility and How Yoga Can Help
Stress is a physiological response to a perceived threat or challenge. It triggers the release of hormones like cortisol and adrenaline, which prepare the body for fight or flight. While this response is helpful in short-term situations, chronic stress can negatively affect health.
Chronic stress can also lead to oxidative stress, which can damage sperm DNA and reduce fertility. By reducing stress through yoga, you're on your way to improving the vitality of your sperm and enhancing fertility.
Yoga Poses and Techniques for Improving Sperm Health Before You Donate
Several yoga poses and techniques can improve sperm health. Some of the most effective poses include the Cobra pose, the Bridge pose, and the Shoulder stand. These poses help to improve blood flow to the reproductive organs, which can increase the production of healthy sperm. Other techniques that can help to improve sperm health include deep breathing exercises, meditation, and visualization.
Tips for Incorporating Yoga into Your Routine Before Donating Sperm
Incorporating yoga into your routine before you donate sperm can greatly improve sperm health and increase the chances of successful insemination when a family or individual purchases your vial. Some practical tips for incorporating yoga into your routine include finding a routine that works for you! We all have busy schedules, but once you begin to take steps toward incorporating a yoga routine, it'll become second nature. To start, try practicing consistently and set aside time each day for yoga practice. Setting the alarm for the times you wish to practice each day will ensure you will remember. It is also essential to listen to your body and avoid overexertion. Drink plenty of water so you're staying hydrated.
Lastly, don't give up on trying to enhance your sperm quality with yoga and other meditation practices! At Cryobank America, we're looking for suitable candidates to donate sperm. When you join our program, you can help a family fulfill their dreams of conceiving while you receive extra income!
Click here for more helpful tips.
Click here to learn about our qualifications and incentives for becoming a donor.
Different Vial Types:
If you have been curious about using sperm donors to help start your family, you may have looked at the prices of vials and noticed several different types available. What is an IUI, ICI, A.R.T., and IVF vial? This blog will let you know the differences between each one so that it can guide you in figuring out which vial is best for you.
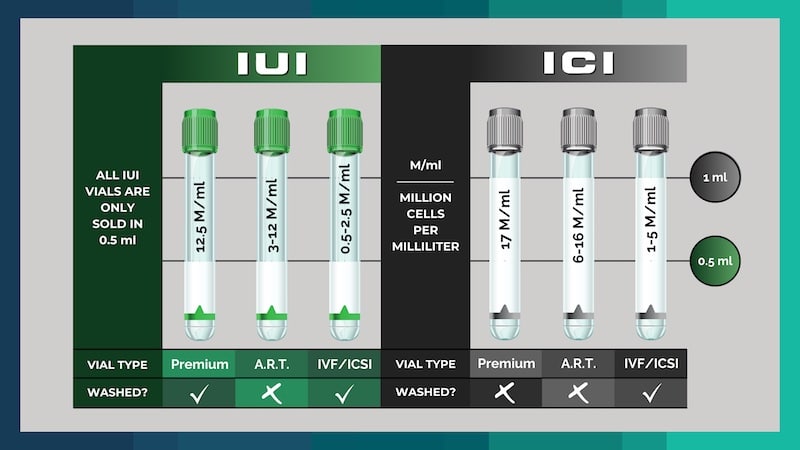
IUI Premium Vials
IUI (Intrauterine insemination) vials undergo a "washing" procedure utilizing gradient separation methods, resulting in only the sperm and stabilizing media, making it safe for the uterus.
At Cryobank America, we guarantee 25 Million cells per milliliter (25M/ml). Each IUI vial is sold in a half-milliliter (0.5ml) unit, giving you 12.5M/ml of motile sperm cells per premium IUI vial. IUI specimens can be safely placed directly into the uterus by your treating physician because there are no "round" cells or other "junk" in them that causes cramping. These units are also ideal for at-home inseminations, where they'll be placed near the top of the vagina and cervix.
ICI Premium Vials
ICI (intracervical insemination) vials are considered "unwashed" since they have not undergone gradient separation steps, which remove the non-motile sperm cells, round cells, and other junk found in the ejaculate.
At Cryobank America, we guarantee 17 Million cells per milliliter (17M/ml). Each vial sold comprises one milliliter (1ml). ICI units are typically used for at-home insemination since these specimens cannot be placed into the uterus due to severe cramping. Some fertility clinics prefer to wash their patient's specimens in-house (usually at an additional cost to the patient); therefore, these units contain one milliliter of a specimen compared to IUI units, which are sold in half milliliter units (0.5ml). We recommend our clients purchase IUI units since they can work for both in-clinic procedures and at-home inseminations and have the highest concentration of motile sperm cells, increasing the chances of successful insemination.
IUI A.R.T. & ICI A.R.T.
A.R.T., or artificial reproductive technology, vials are lower quantity units. At Cryobank America, we guarantee 3-12 Million per half a milliliter (and 6-24 M/ml) for IUI ART and 6-16 M/ml for ICI ART units. These vials cost less since they contain fewer progressively motile sperm cells.
IUI/IVF & ICI/IVF (For IVF/ICSI)
Lastly, our IUI/IVF undergoes our wash process and is guaranteed at 0.5-2.5 Million per half (0.5) milliliter (1-5 M/ml). Our ICI/IVF vials are unwashed, guaranteeing 1-5 Million per (1) milliliter. We recommend these units for clients utilizing in-vitro fertilization or Intracytoplasmic Sperm Injection (ICSI) procedures, where only a few sperm are needed.
If you still have questions concerning vial types and differences between the classes, don't hesitate to contact one of our friendly and knowledgeable Cryobank America staff members today!
Please email us at [email protected] or give us a call at 817-945-8708
All pricing can be found at https://cryobankamerica.com/pricing/
It’s often asked, is there a supplement that could help increase your fertility? There is, and it’s called Coenzyme-10, or CoQ10 for short. This supplement is a natural antioxidant that helps with the defragmentation of sperm and the aging process of oocytes. Essentially, it is keeping your eggs and sperm at a healthy young age, even as you age every day. It doesn’t reverse the aging problems that occur naturally with aging but can help stabilize it and reduce the fragmentation of your sperm, which slows the aging process.
CoQ10’s primary purpose was to help heart function, but over the years, fertility doctors and specialists have figured out that it helps sperm and Oocytes as well. Additionally, research shows CoQ10 may be beneficial for Parkinson’s disease patients, can decrease the frequency of migraine headaches, and can enhance energy production to aid in physical performance. You can pick this up over the counter at a local drug store or pharmacies like CVS, Walgreens, or Walmart. It’s relatively inexpensive and could help you and your partner conceive faster! While CoQ10 is considered safe, you should consult your healthcare provider first with all supplements.
If you are wondering about your fertility and want to learn more about your sperm count, you can find more information HERE on how Cryobank America can help!

