When it comes to starting a family, there are many decisions you must make. One of those decisions is choosing a sperm donor. While this may seem like a straightforward process, it is crucial to prioritize the protection of one's health. There has been increased discussion and visibility of natural insemination (NI) in recent years, mainly due to online platforms and forums that connect individuals seeking sperm donors. While some people may choose natural insemination for various reasons, you should consider this method's potential risks. Opting for a sperm bank and artificial insemination (AI) can increase safety and peace of mind.
Key Takeaways
- Natural insemination carries risks of sexually transmitted infections and unwanted pregnancies.
- Choosing a sperm bank provides quality control measures and screening/testing of donors.
- Donor anonymity and confidentiality are maintained, but recipients can access medical history and donor profiles.
- Legal protections exist for both donors and recipients in the sperm bank process.
- Artificial insemination can provide better chances of pregnancy.
- While cost and accessibility may vary, making an informed decision for your health is crucial.
What is Natural Insemination?
Natural insemination refers to the process of conceiving a child through sexual intercourse with a sperm donor. Unlike sperm banks, natural insemination involves direct contact between the donor and the recipient. While some individuals may prefer this method due to its perceived intimacy, it is essential to consider the potential risks involved.
The Risks of Natural Insemination
When it comes to natural insemination, there are several health risks that both donors and recipients should be aware of. Firstly, there is an increased risk of sexually transmitted infections (STIs) as there is direct contact between the donor and recipient. Additionally, there is a lack of quality control and screening measures in place, which can lead to potential genetic disorders or other health complications for the child.
From a legal standpoint, natural insemination poses risks for both parties. Donors may face unexpected legal responsibilities and obligations towards the child without proper legal agreements. Similarly, recipients may encounter difficulties establishing legal parentage or obtaining financial support from the donor.

The Benefits of Choosing AI Over NI
| Benefit | Assisted Hatching May Benefit: |
| Increased chances of conception | Sperm banks offer a wide selection of healthy and viable sperm, increasing the chances of successful conception. |
| Screened donors | Sperm banks thoroughly screen and test their donors for genetic and infectious diseases, ensuring the safety of the recipient and any resulting offspring. |
| Privacy and anonymity | Sperm banks offer the option to donate anonymously, allowing recipients to maintain their privacy and avoid potential legal or emotional complications. |
| Access to medical history | Sperm banks provide detailed medical histories and updated reports of their donors, allowing recipients to make informed decisions about their choice of donor and potential health risks. |
| Convenient and flexible scheduling | Sperm banks offer flexible scheduling options for donors and recipients, making sperm donation and insemination more convenient and accessible. |
Opting for a sperm bank offers numerous benefits when compared to natural insemination. Firstly, sperm banks provide increased safety and protection for donors and recipients. Sperm samples are thoroughly screened and tested for genetic disorders, infectious diseases, and other health conditions before being made available for use. This rigorous screening process significantly reduces the risk of passing on hereditary diseases or infections to the child.
Furthermore, sperm banks offer access to high-quality sperm from carefully selected donors. Donors undergo extensive screening, including medical and psychological evaluations, to ensure suitability. These screenings ensure that recipients have access to sperm from healthy individuals with desirable genetic traits, increasing the chances of a successful pregnancy.
Quality Control Measures in Sperm Banks That You Won't Get Through Natural Insemination
Sperm banks prioritize quality control measures to ensure the health and safety of recipients. The screening and testing process for sperm donors is comprehensive and stringent. Donors are required to undergo thorough medical examinations, including genetic testing, to identify any potential health risks. Additionally, they receive screenings for infectious diseases such as HIV, hepatitis, and syphilis.
Sperm samples are also subject to strict quality control measures. They are tested for motility, viability, and concentration to ensure their suitability for fertility treatments. By implementing these quality control measures, sperm banks assure recipients that they receive sperm from healthy and viable donors.
Screening and Testing of Donors
The screening and testing process for sperm donors ensures the health and well-being of recipients and their future children. Donors must undergo a series of evaluations to assess their physical and mental health. These evaluations include a comprehensive medical history review, physical examinations, and genetic testing.
Genetic testing is vital in identifying potential hereditary diseases that could affect future children. Donors receive screenings for conditions including cystic fibrosis, sickle cell anemia, and various genetic disorders. By conducting these tests, sperm banks can provide recipients with valuable information about the genetic health of their chosen donor.
Donor Anonymity and Confidentiality
Donor anonymity and confidentiality are essential considerations when choosing a sperm donor. Sperm banks prioritize the protection of donor identities to ensure their privacy. This anonymity allows donors to contribute without fear of future legal or emotional obligations towards the child.
Recipients also benefit from donor anonymity, as it allows them to make decisions about their family without external interference. It will enable them to focus on their desires and preferences when selecting a donor without feeling obligated to establish a relationship with the donor in the future.
Access to Donor Information and Medical History
One of the significant advantages of using a sperm bank is the access recipients have to comprehensive donor information and medical history. Sperm banks maintain detailed profiles for each donor, including physical characteristics, educational background, and personal interests. This information allows recipients to choose a donor who aligns with their preferences and values.
Furthermore, recipients have access to the donor's medical history. This information includes any known or newly developed genetic conditions or family health issues. This information is invaluable in understanding potential health risks for the child and making informed decisions about their future well-being.
Diversity of Donor Profiles
Sperm banks offer an extensive range of donor profiles, ensuring recipients have a diverse selection. Donors come from various ethnic backgrounds, allowing recipients to find a donor who shares their cultural heritage. Diversity is crucial for those who want to preserve their cultural roots or guarantee their offspring will inherit a varied genetic makeup.
The availability of diverse donor profiles also ensures that recipients can find donors who possess specific physical traits or talents they desire for their child. Whether it is eye color, height, or musical abilities, sperm banks provide an extensive selection to cater to individual preferences.
Legal Protections for Donors and Recipients
When using a sperm bank, both donors and recipients are protected by legal frameworks. This framework shields donors from legal responsibilities or obligations towards the child conceived through their donation. Recipients, on the other hand, are provided with legal protections regarding parentage and financial support.
These legal protections provide peace of mind for both parties involved, ensuring they can make decisions about their family without fear of future legal complications or disputes.
Cost and Accessibility of Sperm Banks
While the cost of using a sperm bank may be higher compared to natural insemination, the long-term benefits and peace of mind it provides make it worth the added costs. Sperm banks offer various pricing options, allowing recipients to choose a plan that suits their budget. Additionally, many sperm banks provide financing options to make the process more accessible.
Regarding accessibility, sperm banks have a vast network of locations, making it easier for individuals to access their services. These expansions ensure that individuals from different geographical areas have equal opportunities to choose a suitable donor and start their journey toward parenthood.
Choosing A Sperm Bank Over Natural Insemination For Your Health
Protecting one's health should be a top priority when choosing a sperm donor. While natural insemination may seem appealing due to its perceived intimacy and low costs, it comes with significant risks, both in terms of health and legality. Opting for a sperm bank provides increased safety and protection for both donors and recipients.
Sperm banks implement rigorous quality control measures, including comprehensive screening and testing processes for donors. Testing ensures recipients access high-quality sperm from healthy individuals with desirable genetic traits. Additionally, sperm banks offer valuable donor information and updated medical history, allowing recipients to make informed decisions about their future families.
By choosing a sperm bank over natural insemination, you can ensure optimal health and safety while embarking on parenthood. Making a calculated decision that considers long-term implications and provides the best possible outcome for all parties involved is crucial.
Natural Insemination and Artificial Insemination FAQ
What is a sperm bank?
A sperm bank is a facility that collects, freezes, and stores sperm from donors for use in artificial insemination procedures, such as IUI, ICI, IVF, ICSI, and home insemination.
What are the benefits of choosing a sperm bank over natural insemination?
Choosing a sperm bank over natural insemination can provide several benefits. These benefits include access to a wide range of donors, increased control over the selection process, and reduced risk of sexually transmitted infections and passing on genetic conditions.
Does natural insemination have a higher success rate than artificial insemination?
No scientific evidence suggests that natural insemination's success rate is higher than artificial insemination. Artificial insemination techniques have been developed and refined over many years to maximize the chances of successful conception. They allow for controlled and precise placement of sperm, which can increase the likelihood of fertilization.
Is using a sperm bank more expensive than natural insemination?
The cost of natural insemination can vary depending on the donor and the specific arrangement. Some NI donors may offer their services for free, while others may charge a fee. Using a sperm bank can be expensive, with costs ranging from $500 to $10,000 per cycle. However, many insurance plans cover the costs of fertility treatments, and many sperm banks offer financing options.
Can I choose the physical characteristics of the sperm donor?
Many sperm banks provide childhood and adult photos of each donor, allowing recipients to select donors based on physical characteristics. They also offer photo-matching services so recipients can choose a donor that closely resembles their physical traits.
Is using a sperm bank safe?
Using a reputable sperm bank is safe. They are regulated and inspected by the Food and Drug Administration (FDA) and Clinical Laboratory Improvement Amendments (CLIA) to ensure optimal safety. Additionally, sperm is stored and handled in a controlled environment to prevent the risk of contamination or infection.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Choosing IUI, ICSI, or At-Home Insemination Over IVF: 4 Factors You Should Know
Exploring different fertility treatment options requires a deep understanding of various factors, ranging from medical to financial, to personal preferences. While In-Vitro Fertilization (IVF) is undoubtedly one of the most recognized fertility treatments, other methods like Intrauterine Insemination (IUI), Intracytoplasmic Sperm Injection (ICSI), and at-home insemination have their unique appeal and benefits. But what drives the decision to choose one over the other? Here, we delve into the reasons.
1. Choosing IVF For Fertility Health and Specific Challenges
The first and foremost consideration is the specific fertility challenge a couple or individual is facing. While IVF is robust and addresses a wide array of fertility issues, some challenges may be addressed more directly with other treatments.
Male Infertility Issues
ICSI, a specialized form of IVF, has emerged as a game-changer for couples dealing with male infertility. By directly injecting a single healthy sperm into an egg, it bypasses challenges like low sperm count or poor sperm mobility. Thus, for those who have identified male infertility as the primary obstacle, ICSI might be a more direct solution than traditional IVF.
Uncomplicated Infertility Or Use Of Donor Sperm
For women with open fallopian tubes, regular ovulation, and no apparent severe infertility issues, IUI provides a less invasive approach. It's particularly popular among single women or lesbian couples using donor sperm.
2. Choosing IUI Or At-Home Insemination Due To Financial Considerations
Fertility treatments can be expensive, and not everyone has the luxury of unlimited resources or comprehensive insurance coverage.
Which Procedure Is Less Expensive, IUI or IVF?
Generally, IUI is less expensive than IVF or ICSI. For those who are on a tighter budget, starting with IUI might be a feasible first step. If several IUI cycles don't result in pregnancy, they might then consider investing in IVF or ICSI.
Cumulative Costs — What's Really More Expensive, IUI or IVF?
It's also essential to consider cumulative costs. While IUI per cycle might be cheaper, if multiple cycles are needed, the costs can add up. In contrast, IVF, though pricier upfront, might offer a higher success rate per cycle. The bottom line will be determined by your overall fertility health, donor or partner compatibility, and timing insemination correctly by precisely tracking your ovulation cycle.
Many cryobanks offer financial services such as payment plans and financing. Cryobank America has partnered with Future Family to offer patients affordable financing options.

3. Choosing IUI, IVF, or At-Home Insemination For Personal Preferences and Comfort
Medical procedures, even if they're routine from a clinical perspective, are deeply personal experiences.
Invasiveness and Comfort — IUI
IUI stands distinct with its simplicity. By directly introducing sperm into the uterus, it bypasses many of the steps intrinsic to IVF, such as egg retrieval and external fertilization. This straightforwardness can be less daunting for those who are apprehensive about medical procedures. The very nature of IUI, being less invasive, can also mean reduced physical discomfort, fewer side effects, and a shorter recovery period.
For many, starting with IUI is a gentle introduction to fertility treatments. The rationale often revolves around giving the less invasive method a try first, hoping it might lead to successful conception without the need for more complex procedures.
Natural Conception
Fertility treatments, for all their medical advancements, can sometimes feel clinical and detached from the intimate experience of conception. This feeling can be a significant determinant in the choices couples make. There's an inherent appeal in procedures that mimic or come close to the process of natural conception.
IUI, especially when executed without the aid of fertility drugs, offers an experience that's remarkably close to natural conception. The process aligns with the body's natural ovulation cycle, and the sperm is introduced directly into the uterus without any external fertilization. This method provides couples with a sense of familiarity and naturalness, making the journey feel less 'medical' and more intimate.
At-Home Insemination
The appeal of at-home insemination lies in its intimacy and privacy. For those who find clinical settings stressful or impersonal, at-home insemination offers a more comfortable and familiar environment. This method is also more cost-effective than clinical procedures, though it may have a lower success rate and lacks the oversight and expertise of a medical setting.
4. Treatment Duration and Timelines
For some, the time it takes from starting treatment to achieving pregnancy is a significant factor.
Which Procedure Is Quicker, IUI or IVF?
IUI stands out as a relatively quicker procedure when juxtaposed against IVF (in vitro fertilization). The simplicity of IUI, which involves directly introducing sperm into the uterus, eliminates several steps intrinsic to the IVF process, such as egg retrieval and lab fertilization. For those already navigating the emotionally charged waters of fertility challenges, the shorter treatment duration of IUI can be a breath of fresh air. It offers hope without the extended commitment, making it an attractive choice for those wary of prolonged medical interventions.
Does IUI or IVF Have A Higher Success Rate?
Time considerations in fertility treatments aren't just about the procedure's speed. It's also about effectiveness across multiple cycles. Here's where the dynamics become intricate. IVF, despite its lengthier process, often touts a higher success rate per cycle when compared to IUI. This statistic can translate to fewer overall treatment cycles, potentially shortening the entire duration from the start of treatment to conception.
On the flip side, the non-invasiveness, simplicity, and lower immediate costs of IUI can lead some to opt for multiple IUI cycles before considering the switch to IVF. The thought process here hinges on hope: the hope that the next IUI cycle might be a successful one, coupled with the procedure's relative simplicity.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Comparing IVF, ICSI, and IUI: Understanding Your Options in Fertility Treatments
Embarking on the path to parenthood, many couples and individuals find themselves at the crossroads of fertility treatments. The journey, while filled with hope, often presents a maze of medical terms, techniques, and decisions. The options — IVF, ICSI, and IUI — though different, all aim to assist in the realization of the dream of having a child. Delving deeper into each method helps demystify the process and sheds light on the complications involved.
Please make sure to also contact a suitable health professional. While this article is your information guide, it is not to be used as a substitute for medical opinion or healthcare treatment.
IVF (In-Vitro Fertilization)
IVF involves stimulating the ovaries using fertility drugs to produce mature eggs. These eggs are then retrieved and fertilized in a lab with sperm from a partner or a donor. The resultant embryo is monitored for signs of fertilization, and the best-quality embryo is transferred to the uterus.
Advantages of IVF
IVF is a comprehensive treatment that can address both male and female infertility factors. Through IVF, mature eggs are retrieved and fertilized in a laboratory setting, and the best-quality embryos are chosen for transfer, increasing the chances of success. The process allows for advanced embryo selection techniques, such as time-lapse monitoring and Preimplantation Genetic Screening. This ensures only embryos with the highest potential are selected. IVF provides the flexibility to use either a partner's or a donor's sperm, giving diverse options for family planning. Additionally, if more than one high-quality embryo results from the cycle, the extra embryos can be frozen for future use.
When is IVF advised?
IVF is typically recommended for those with fallopian tube damage, blockages, or in cases of unexplained infertility. It's also a viable option in mild cases of male infertility.
ICSI (Intracytoplasmic Sperm Injection)
ICSI (Intracytoplasmic Sperm Injection), on the other hand, is a refined version of IVF. Instead of allowing sperm to fertilize the egg naturally in a dish, ICSI involves the direct injection of a single, chosen sperm into the egg. This technique proves invaluable, especially in cases where male infertility is a concern. By bypassing many natural challenges, ICSI offers a chance even when sperm count is low or mobility is compromised.

Advantages of ICSI
ICSI is a specialized form of IVF where a single, healthy sperm is injected directly into the egg. This direct approach maximizes the chance of fertilization, especially in cases of male infertility. Since only the best quality sperm is selected and used, it ensures the highest potential for successful fertilization. ICSI is particularly beneficial when there are significant sperm problems, such as a low sperm count, poor sperm mobility, or high levels of DNA damage in the sperm. Even when sperm needs to be surgically retrieved, ICSI can still be applied. By addressing male fertility issues directly, ICSI bypasses many obstacles that can prevent natural fertilization.
When is ICSI advised?
ICSI is commonly prescribed for those with male fertility problems such as low sperm count, poor sperm mobility, or high levels of DNA damage in sperm. If male fertility isn't the primary issue, IVF is usually the suggested method.
IUI (Intrauterine Insemination)
IUI (Intrauterine Insemination) stands apart from the aforementioned methods. It is less invasive and mirrors the process of natural conception more closely. In this procedure, prepared sperm is directly introduced into the uterus, timed with ovulation, to facilitate fertilization. For many, IUI serves as a starting point in their fertility journey, especially when the primary concern is not related to sperm quality or quantity.
Advantages of IUI
IUI is a straightforward, non-invasive procedure without the need for anesthesia. It's generally more affordable than advanced fertility treatments such as IVF or ICSI. The entire IUI process can be completed within minutes, making it a quick and hassle-free option. The sperm "washing" process ensures that only the best and healthiest sperm are used for insemination. The timing of the insemination is carefully synchronized with the woman's ovulation to increase the chances of success. IUI can effectively address a range of infertility issues, from unexplained infertility to mild male factor problems. It's also a preferred method when using donor sperm, offering a simpler path for diverse family planning. Unlike some other treatments, there's no need for egg retrieval or surgical intervention, making it less physically demanding.
When is IUI advised?
IUI is an option for patients requiring donor sperm. To succeed, it requires clear fallopian tubes, a healthy sperm count, and a mature egg. In cases of irregular ovulation, fertility drugs may be combined with IUI.
Which Treatment is Right for You?
Your unique fertility situation will determine the best treatment. A comprehensive assessment considering your medical history, age, and response to previous treatments is necessary. For some, IUI might be the first step. However, if significant sperm disorders are detected, IVF or ICSI might be more suitable.
It's essential to understand that your fertility journey is individual. The goal is to achieve pregnancy in the most efficient and effective manner. Always ensure that you are part of the decision-making process, aware of the costs, and fully informed about the treatment path ahead.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is ICSI and How Does it Work?
ICSI, or intracytoplasmic sperm injection, is a fertility treatment that involves the direct injection of a single sperm into an egg. This procedure is performed with in vitro fertilization (IVF). During IVF, eggs are retrieved from the woman's ovaries and fertilized with sperm in a laboratory dish. With ICSI, a single sperm is selected and injected directly into each egg, bypassing any potential barriers to fertilization.
The ICSI procedure begins with collecting eggs from the woman's ovaries. These eggs are then placed in a culture dish and examined under a microscope. A single sperm is selected and immobilized using a tiny needle. The needle injects the sperm directly into the egg. After the injection, monitoring the eggs ensures that fertilization occurs. Once fertilization is confirmed, the resulting embryos transfer to the woman's uterus.
Compared to other fertility treatments, such as IVF alone, ICSI offers a higher chance of successful fertilization. This procedure is particularly beneficial for couples who have struggled with male factor infertility, where the quality or quantity of sperm may be compromised due to various factors. ICSI can be helpful in cases where previous attempts at IVF have failed or when there are concerns about the ability of the sperm to penetrate the egg.
Who is a Candidate for ICSI?
Several factors may lead to the need for ICSI.
Male factor infertility is one of the most common reasons for considering ICSI. These factors include low sperm count, poor sperm motility, or abnormal sperm morphology. ICSI can also benefit couples who have experienced previous failed attempts at IVF or have had difficulty achieving fertilization with conventional IVF methods.
Medical Conditions and ICSI
In addition to male factor infertility, certain medical conditions may affect a couple's candidacy for ICSI. These include genetic disorders that are likely to get passed on to offspring, such as cystic fibrosis or Huntington's disease. ICSI can be used with preimplantation genetic testing to screen embryos for these conditions before being transferred to the uterus.
Age Requirements For ICSI
Age can also play a role in determining whether a couple is a good candidate for ICSI. As women age, their ovarian reserve decreases, making achieving successful fertilization and pregnancy more difficult. ICSI can help overcome some of these challenges by directly injecting sperm into the egg, increasing the chances of fertilization.
Preparing for ICSI: What to Expect
Before undergoing ICSI, couples typically have an initial consultation with a fertility specialist. During this consultation, the couple's fertility specialist will review their medical history and discuss any potential factors that may affect the success of ICSI. The fertility specialist may also order additional tests and evaluations to assess the couple's health and fertility potential.
Testing and Evaluations
Medical tests and evaluations may include blood tests to check hormone levels, ultrasounds to evaluate the woman's ovarian reserve and uterine health, and semen analysis to assess the quality and quantity of sperm. These tests will help the fertility specialist determine the most appropriate treatment plan for the couple.
Medications and Injections
In preparation for ICSI, the woman may be prescribed medications to stimulate her ovaries and promote the development of multiple eggs. These medications are generally administered through injections, and the fertility clinic will closely monitor progress and any side effects. The fertility specialist will also advise the woman to make specific lifestyle changes, such as quitting smoking, reducing alcohol consumption, and maintaining a healthy diet and exercise routine.

The ICSI Procedure: Step-by-Step
The ICSI procedure typically follows a specific timeline of events. First, the woman will undergo ovarian stimulation using medications to promote the development of multiple eggs. This step is essential to increase the chances of successful fertilization and pregnancy. During this time, the woman will be closely monitored through ultrasounds and blood tests to assess the growth and maturity of the eggs.
Once the eggs have reached the desired size and maturity, retrieval occurs through a minor surgical procedure called egg retrieval. This procedure is performed under sedation or anesthesia and involves the insertion of a needle into the ovaries to collect the eggs. The eggs are then placed in a culture dish and examined under a microscope.
Next, an embryologist selects a single sperm for each egg. The embryologist carefully examines the sperm under a microscope and chooses the healthiest and most viable sperm for injection. The selected sperm is immobilized using a tiny needle and injected directly into the egg.
After the injection, the eggs are monitored to ensure that fertilization occurs. The presence of two pronuclei confirms successful fertilization. The fertilized eggs, now called embryos, are cultured in the laboratory for a few days before being transferred to the woman's uterus.
Success Rates of ICSI: What to Expect
The success rates of ICSI can vary depending on several factors, including the age of the woman, the quality of the eggs and sperm, and the overall health of the couple. Generally, the success rates of ICSI are comparable to those of conventional IVF, but ICSI can improve your success rate.
Factors that may affect the success rates of ICSI include the woman's age and ovarian reserve. As women age, their ovarian reserve decreases, making achieving successful fertilization and pregnancy more difficult. However, ICSI can help overcome some of these challenges by directly injecting sperm into the egg, increasing the chances of fertilization.
A fertility specialist should discuss realistic expectations during the initial consultation. The fertility specialist can provide personalized guidance based on the individual or couple's circumstances and help manage expectations throughout treatment.
It is also important to note that success rates can vary between fertility clinics. When choosing a fertility clinic for ICSI, it is essential to consider the clinic's success rates and the qualifications and experience of the medical team. A qualified and experienced team can significantly increase the chances of a successful outcome.
After the Procedure: What to Expect
After the ICSI procedure, the woman will typically have a recovery period of a few days. During this time, she may experience discomfort or bloating as her body adjusts to the hormonal changes. A doctor can prescribe pain medication to help manage any discomfort.
A fertility specialist will schedule follow-up appointments to monitor the woman's progress and assess the procedure's success. These appointments may include ultrasounds and blood tests to check for pregnancy and monitor embryo development.
Emotional and psychological considerations are also necessary after the ICSI procedure. Infertility can affect an individual or couple's mental health, and it is crucial to seek support and counseling if needed. Many fertility clinics offer counseling services or can provide referrals to mental health professionals who specialize in infertility.
Alternative Fertility Treatments to Consider
While ICSI is a highly effective fertility treatment, it may not be the right option for every couple. There are several alternative treatments that couples struggling with infertility may consider.
One alternative treatment is intrauterine insemination (IUI), which involves placing sperm directly into the woman's uterus during ovulation. IUI can be a less invasive and less expensive option for couples with mild male factor infertility or unexplained infertility.
In some cases, a fertility specialist may suggest gestational surrogacy. Gestational surrogacy involves using a surrogate to carry the pregnancy for the couple or individual. This process can be an option for couples where the woman cannot carry a pregnancy due to medical reasons.
It is essential for couples and individuals to thoroughly discuss their options with a fertility specialist to determine the most appropriate treatment plan for their specific circumstances.
Choosing the Right Fertility Clinic for ICSI
Choosing the right fertility clinic for ICSI is crucial for a successful outcome. There are several factors to consider when making this decision.
First and foremost, choosing a fertility clinic with a qualified and experienced team is essential. The fertility specialists should have extensive ICSI experience and be board-certified in reproductive endocrinology and infertility.
The success rates of the fertility clinic should also be considered. The clinic should have a track record of high success rates, particularly in cases similar to the couple's specific circumstances.
The clinic's facilities and laboratory should also be state-of-the-art and equipped with the latest technology and equipment. These elements will ensure that the ICSI procedure is performed under optimal conditions.
During the initial consultation with the fertility clinic, asking questions and gathering as much information as possible is essential. This information can include questions about the clinic's success rates, the qualifications and experience of the medical team, and the specific steps and timeline of the ICSI procedure.
Choosing the right fertility clinic can significantly increase the chances of a successful outcome and provide couples with the support and guidance they need during this challenging time.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
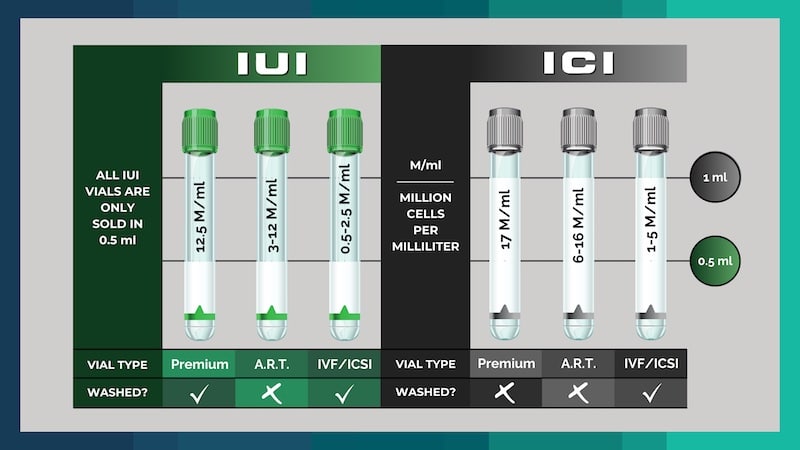
Different Vial Types:
If you have been curious about using sperm donors to help start your family, you may have looked at the prices of vials and noticed several different types available. What is an IUI, ICI, A.R.T., and IVF vial? This blog will let you know the differences between each one so that it can guide you in figuring out which vial is best for you.
IUI Premium Vials
IUI (Intrauterine insemination) vials undergo a "washing" procedure utilizing gradient separation methods, resulting in only the sperm and stabilizing media, making it safe for the uterus.
At Cryobank America, we guarantee 25 Million cells per milliliter (25M/ml). Each IUI vial is sold in a half-milliliter (0.5ml) unit, giving you 12.5M/ml of motile sperm cells per premium IUI vial. IUI specimens can be safely placed directly into the uterus by your treating physician because there are no "round" cells or other "junk" in them that causes cramping. These units are also ideal for at-home inseminations, where they'll be placed near the top of the vagina and cervix.
ICI Premium Vials
ICI (intracervical insemination) vials are considered "unwashed" since they have not undergone gradient separation steps, which remove the non-motile sperm cells, round cells, and other junk found in the ejaculate.
At Cryobank America, we guarantee 17 Million cells per milliliter (17M/ml). Each vial sold comprises one milliliter (1ml). ICI units are typically used for at-home insemination since these specimens cannot be placed into the uterus due to severe cramping. Some fertility clinics prefer to wash their patient's specimens in-house (usually at an additional cost to the patient); therefore, these units contain one milliliter of a specimen compared to IUI units, which are sold in half milliliter units (0.5ml). We recommend our clients purchase IUI units since they can work for both in-clinic procedures and at-home inseminations and have the highest concentration of motile sperm cells, increasing the chances of successful insemination.
IUI A.R.T. & ICI A.R.T.
A.R.T., or artificial reproductive technology, vials are lower quantity units. At Cryobank America, we guarantee 3-12 Million per half a milliliter (and 6-24 M/ml) for IUI ART and 6-16 M/ml for ICI ART units. These vials cost less since they contain fewer progressively motile sperm cells.
IUI/IVF & ICI/IVF (For IVF/ICSI)
Lastly, our IUI/IVF undergoes our wash process and is guaranteed at 0.5-2.5 Million per half (0.5) milliliter (1-5 M/ml). Our ICI/IVF vials are unwashed, guaranteeing 1-5 Million per (1) milliliter. We recommend these units for clients utilizing in-vitro fertilization or Intracytoplasmic Sperm Injection (ICSI) procedures, where only a few sperm are needed.
If you still have questions concerning vial types and differences between the classes, don't hesitate to contact one of our friendly and knowledgeable Cryobank America staff members today!
Please email us at [email protected] or give us a call at 817-945-8708
All pricing can be found at https://cryobankamerica.com/pricing/

