What is CMV?
CMV, cytomegalovirus, is a member of the herpesvirus family and is highly prevalent worldwide. You can become infected with CMV through bodily fluids, including saliva, urine, blood, seminal fluid, and breast milk. The most common transmission modes are through close contact with infected individuals or exposure to bodily fluids. It is important to note that CMV can be present in an individual's body without causing any symptoms or illness, making detecting and preventing transmission challenging.

How Common is CMV?
The CDC states that nearly 1 in 3 children have already been infected with CMV by age 5, and by the age of 40, over half of the population is infected. The prevalence of CMV in sperm donors varies depending on the screened population. Studies have shown that CMV infection rates among sperm donors range from 30% to 70%. However, it is essential to note that the presence of CMV does not necessarily indicate active infection or the potential for transmission. Donor screening protocols typically include testing for CMV antibodies, which can help determine if the donor has contacted the virus in the past.
Symptoms of CMV Infection
CMV infection can manifest differently in individuals depending on their immune system and overall health. Many people infected with CMV may not experience symptoms or only have mild symptoms that resolve independently. However, those with weakened immune systems, such as individuals with HIV/AIDS or undergoing organ transplantation, may develop severe complications. These can include pneumonia, hepatitis, retinitis (inflammation of the retina), and neurological disorders. Awareness of these symptoms and seeking medical attention if necessary is crucial.
Becoming Infected With CMV
Primary CMV infection occurs in people who have never been exposed to the CMV virus before. Once a person becomes infected with CMV, the virus remains alive but dormant inside their body for the rest of their life. Recurrent CMV infection is when a dormant virus becomes active again. CMV infection is usually harmless and rarely causes illness. However, primary CMV infection can cause more severe problems for pregnant women than recurrent CMV infection.
Cytomegalovirus
CMV in human cells.
Diagnosis and Treatment of CMV Infection
Diagnosing CMV infection involves various methods, including blood tests to detect the presence of CMV antibodies or viral DNA. Other tests like urine or saliva samples may also confirm active infection. Treatment options for CMV infection depend on the severity of symptoms and the individual's immune status. A healthcare provider may prescribe antiviral medications to manage the condition and reduce the risk of complications.
Prevention of CMV Transmission in Sperm Donation
Preventing CMV transmission in sperm donation involves following proper protocols and procedures. Donor screening for CMV antibodies is essential in identifying potential donors who may pose a higher risk of transmission. Additionally, implementing strict guidelines for handling and processing donated sperm can help minimize the risk of contamination. Cryopreservation techniques, such as freezing and quarantine periods, can also be employed to ensure that donated sperm is free from infectious agents before use.
CMV Protocols At Cryobank America
The FDA requires CMV testing on all men who intend to donate sperm. A positive result, however, doesn't necessarily mean that a man will be ineligible to donate. Cryobank America will obtain semen samples from potential donors and then quarantine those specimens for at least six months. During that time, the donor may have had CMV antibody levels tested several times. If the antibody tests indicate the possibility of a CMV infection close to the time of the sperm donation, the donor will not be allowed to donate their specimens. If the testing demonstrates inconclusive results, the donor will not be permitted to donate. However, if a donor tests positive for CMV IgG only, indicating a past infection, he will be eligible to contribute. These samples appear in the Cryobank America donor database as CMV-positive.
Can Washed Donor Sperm Transmit CMV?
No, clinically washed sperm is typically free from CMV (Cytomegalovirus) transmission. The sperm-washing process separates sperm from the seminal fluid, which reduces the risk of transmitting infections such as CMV. However, no medical procedure can guarantee 100% elimination of all viruses or infections. You should always consult a healthcare professional for personalized advice and information.
Considering Pregnancy Through Donor Sperm?
Women considering pregnancy with donor sperm should have CMV antibody testing as part of their IDT. Those with a past infection are at low risk of transmitting CMV infection to a fetus and are at little to no risk if they decide to use a CMV-positive donor.
Women never exposed to CMV should consider using a CMV-negative donor. Even though the risk from a CMV-positive donor is low, it is impossible to determine whether there will be a risk for infection.
Cryobank America's donor catalog has a CMV search filter for positive and negative sperm donors. To find a CMV-negative sperm donor, select negative under the CMV option!
CMV Resources
For additional information on CMV, this link is especially helpful:
https://www.mayoclinic.org/diseases-conditions/cmv/symptoms-causes/syc-20355358
If you have any questions about CMV, please email us at [email protected] or call 817-945-8708; we will be happy to help!
The Primary Components of Sperm
Sperm is a fluid that results from ejaculation from the penis during sexual intercourse. It is composed of various components, each serving a specific function. Learn about the details of sperm, what each element consists of, and their essential functions.
Secretion From The Cowper's Glands
The secretion from the Cowper's glands, also known as bulbourethral glands, is a clear, viscous fluid. It contains mucus and various enzymes, such as prostate-specific antigen (PSA), which helps to neutralize the acidity of the urethra and lubricate the passage for sperm during ejaculation.
Other enzymes in this secretion include:
1. Mucin: It is a glycoprotein that helps in lubricating the urethra and facilitates the passage of semen during ejaculation.
2. Proteolytic enzymes: These enzymes help in breaking down proteins present in the semen, which aids in liquefaction of the ejaculate.
3. Acid phosphatase: It is an enzyme that helps in maintaining the acidic pH of the semen, which is vital for sperm function and survival.
4. Fibrinolysin: This enzyme helps break down fibrin, a protein involved in blood clotting. Its presence in the Cowper's gland secretion helps to prevent the clotting of semen within the urethra.
These enzymes collectively contribute to the composition and function of the Cowper's gland secretion during sexual arousal and ejaculation.
PSA (Prostate-Specific Antigen) In Sperm
PSA (Prostate-Specific Antigen) is an enzyme that helps to liquefy sperm, allowing it to become more fluid and mobile. Liquefaction plays a crucial role in facilitating the mobility and viability of sperm cells as they navigate through the female reproductive system.
PSA is tested to check for prostate cancer because it is a protein produced by the cells of the prostate gland. Elevated levels of PSA in the bloodstream may suggest the existence of prostate cancer or other prostate-related ailments, such as prostatitis or benign prostatic hyperplasia (BPH). However, it is essential to note that an elevated PSA level does not necessarily mean a person has prostate cancer, as other factors can also cause PSA levels to rise. Therefore, PSA testing serves as an initial screening tool to identify whether an individual needs further evaluation for prostate cancer.
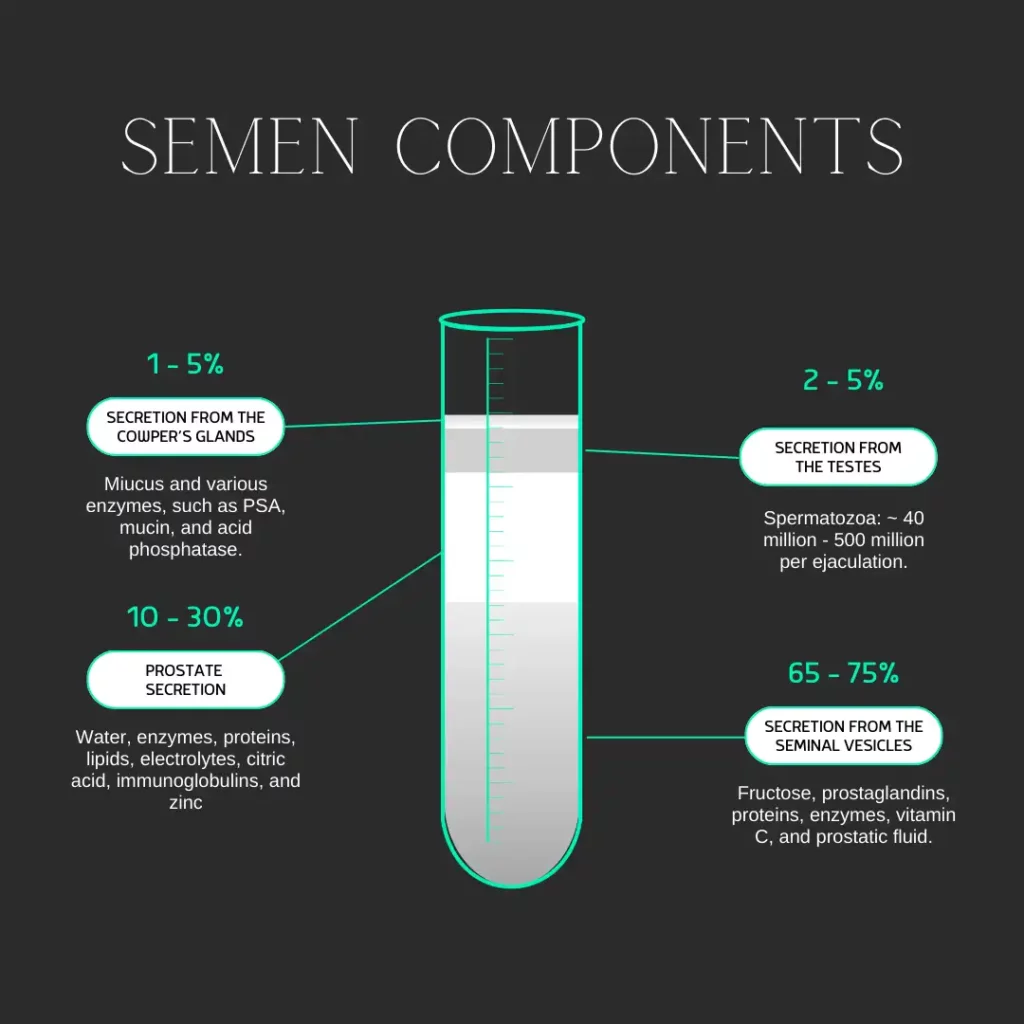
Secretion From The Testes
The secretion from the testes primarily consists of sperm cells and various hormones, including testosterone, dihydrotestosterone (DHT), and inhibin.
Spermatozoa (Sperm Cells)
Spermatozoa, also known as sperm cells, are the reproductive cells produced in the testes. They are responsible for fertilizing the female egg during sexual reproduction. The number of sperm cells produced in the testes and released during one ejaculation can vary. The testes produce around 100 million to 300 million sperm cells daily. However, during ejaculation, the number of sperm cells released is typically much lower.
A typical ejaculation can release anywhere from 40 million to 500 million sperm cells. Some ejaculates may contain more than a billion cells. The number can depend on overall health, age, and sexual activity.
Testosterone In Sperm
Testosterone, the primary male sex hormone, is secreted from the testes. It plays a pivotal role in maintaining and producing male reproductive tissues and secondary sexual characteristics. Testosterone stimulates the growth and development of the male reproductive organs, including the testes, prostate gland, and seminal vesicles. It also promotes the production of sperm cells in the testes.
Apart from its crucial role in male reproductive function, testosterone also impacts a range of other physiological processes in males. It helps regulate muscle mass and strength, bone density, and red blood cell production. Testosterone is also involved in maintaining libido (sex drive) and regulating mood and cognitive function.
Overall, testosterone is essential for the proper functioning of male reproductive organs and has a significant impact on various aspects of male physiology and behavior.
DHT
Dihydrotestosterone (DHT) is a hormone predominantly synthesized in the testes and plays a pivotal role in the establishment and sustenance of male sexual traits. DHT is accountable for the growth and maturation of the male reproductive system, encompassing the penis, scrotum, and prostate gland. Furthermore, it aids in developing secondary sexual characteristics, such as facial and body hair growth, muscle mass, and deepening of the voice. Moreover, DHT is instrumental in regulating libido and contributes to sperm production.
Inhibin
Inhibin is a hormone secreted by the Sertoli cells in the testes. It plays a role in the negative feedback regulation of the hypothalamic-pituitary-gonadal axis (a complex hormonal system that regulates reproductive function in both males and females). Inhibin inhibits the secretion of follicle-stimulating hormone (FSH) from the anterior pituitary gland. By suppressing FSH secretion, inhibin helps regulate spermatogenesis and maintain optimal testosterone levels in the testes.
Prostate Secretion In Sperm
Prostate secretion is composed of several components, including:
1. Water: Most prostate secretions are water, which helps dilute and transport other components.
2. Enzymes: The prostate gland produces several enzymes, including prostate-specific antigen (PSA), which helps to liquefy semen after ejaculation.
3. Proteins: Prostate secretion contains various proteins, such as prostate-specific acid phosphatase (PSAP) and prostate-specific membrane antigen (PSMA), which regulate cell growth and function.
4. Lipids: Prostate secretion contains lipids, including cholesterol and fatty acids, which help to maintain the integrity of the cell membranes and provide energy.
5. Electrolytes: The prostate gland secretes a variety of electrolytes, including sodium, potassium, calcium, and magnesium, that play a crucial role in regulating fluid balance within the body.
6. Citric acid: The prostate gland produces citric acid, which helps to provide energy for sperm motility.
7. Zinc: Prostate secretion contains high levels of zinc, which is important for maintaining prostate health and function.
8. Immunoglobulins: Prostate secretion contains immunoglobulins, such as IgA and IgG, which help to protect against infections and maintain immune function in the reproductive system.
Each component works together to nourish and protect sperm cells during ejaculation.
Secretion From The Seminal Vesicles
The seminal vesicles, located behind the bladder in males, are a vital pair of small glands that play a crucial role in producing semen. This fluid serves as a carrier for sperm during ejaculation. The components of seminal vesicles in semen include:
1. Fructose: Seminal vesicles produce fructose, a type of sugar that provides energy for sperm cells.
2. Prostaglandins: These are hormone-like substances that help in the contraction of the female reproductive tract, aiding in sperm movement towards the egg.
3. Proteins and enzymes: Seminal vesicles secrete various proteins and enzymes, including fibrinogen, prostate-specific antigen (PSA), and different proteolytic enzymes. These substances help in the coagulation and liquefaction of semen.
4. Vitamin C: Seminal vesicles also contribute vitamin C to semen, which helps protect sperm cells from oxidative damage.
5. Prostatic fluid: While not directly produced by the seminal vesicles, prostatic fluid is often mixed with seminal vesicle secretions to form semen. The prostatic fluid contains enzymes, citric acid, zinc, and other substances that nourish and protect sperm cells.
Overall, the components produced by seminal vesicles play crucial roles in providing energy to sperm cells, aiding their movement through the female reproductive tract, and protecting them from oxidative damage.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Freezing and Storing Sperm
Sperm freezing is a way for men to save their fertility by freezing and storing their sperm for later use. This technique has become increasingly popular as more individuals recognize the importance of maintaining their reproductive options.
It involves collecting a sperm sample from the individual and subjecting it to a series of steps that prepare it for freezing. A cryobank can store frozen sperm for many years. This storage option allows people to preserve their ability to have children. It benefits those who do not want to start a family immediately.
The history of sperm storage dates back to the 1950s when researchers began experimenting with freezing sperm. Over the years, advancements in technology and techniques have made the process more efficient and successful. Today, sperm storage is a widely accepted method for preserving fertility. Individuals who must undergo cancer treatments or individuals with medical conditions that may affect their fertility also use this method.
The Process of Freezing Sperm
The process of freezing sperm involves several steps to ensure the usability and longevity of the sperm. Once the sample is collected through masturbation, the quality and quantity of the sperm is analyzed.
After the collection and analysis, a cryoprotectant solution is added to the sample. This solution helps protect the sperm from damage during the freezing process. The mixture is divided into small vials or straws labeled and sealed for freezing.
The freezing process typically involves slowly lowering the temperature of the sperm sample to -196 degrees Celsius using liquid nitrogen. This rapid freezing technique is called vitrification.
Vitrification: Rapid Freezing Process
The process of vitrification involves several steps. First, the cells or tissues are treated with a cryoprotectant solution to dehydrate and protect them from freezing damage. Next, they are rapidly cooled to very low temperatures using liquid nitrogen or another cryogenic agent. The rapid cooling prevents the formation of ice crystals and instead forms a glass-like solid.
During vitrification, it is crucial to minimize the exposure of cells or tissues to toxic levels of cryoprotectants. A stepwise approach, where the concentration of cryoprotectants is gradually increased before vitrification, can avoid these harmful levels.
Vitrified samples stored at ultra-low temperatures remain without significant degradation. They can be rapidly thawed and rehydrated for transplantation or research purposes.
Various applications utilize vitrification. Some of these applications include the storage of embryos for in vitro fertilization (IVF), cord blood stem cells, and biological samples for research.
Benefits of Sperm Storage
Sperm storage offers several benefits to individuals who wish to preserve their fertility. One of the primary benefits is the ability to maintain reproductive options in the future. By freezing their sperm, individuals can ensure they have viable sperm available when they are ready to start a family.
Another benefit of sperm storage is the convenience and flexibility it provides. Individuals can freeze their sperm anytime, allowing them to plan for their future without the pressure of starting a family immediately. Storing sperm can benefit individuals pursuing education, career advancement, or other personal goals before beginning a family.
Additionally, sperm storage can reduce the risk of genetic abnormalities in offspring. Freezing sperm at a younger age is very beneficial. It allows individuals to preserve their sperm when it is healthier and less likely to have congenital abnormalities. Storing fertility can be vital for individuals with genetic conditions or a family history of genetic disorders.
Who Can Benefit from Sperm Storage?
Sperm storage can benefit many individuals at risk of fertility loss. It's a smart choice for those who wish to preserve their reproductive options. Some of the groups that can benefit from sperm storage include:
- Certain medical conditions, such as testicular cancer, leukemia, or autoimmune diseases, can affect sperm production or quality. By freezing their sperm before treatment, these individuals can preserve their fertility and increase their chances of having biological children.
- Men undergoing cancer treatment: Chemotherapy and radiation therapy can harm sperm production and quality. Sperm storage before cancer treatment can allow men to have biological children after completing their treatment.
- Men in high-risk occupations exposed to hazardous environments or substances may be at risk of fertility loss. By freezing their sperm, these individuals can protect their fertility and have the option to start a family.
- Men with low sperm counts or poor sperm quality may have difficulty conceiving naturally. By freezing their sperm, they can increase their chances of successful fertilization through assisted reproductive techniques.

Longevity of Frozen Sperm
The longevity of frozen sperm depends on several factors. Storage conditions and the quality of the sperm at the time of freezing are two primary factors. Generally, cryobanks can store frozen sperm for many years without significant loss of viability.
The recommended storage duration for frozen sperm varies depending on the country and the specific regulations in place. In some countries, cryobanks can store frozen sperm for up to 10 years. In other countries, cryobanks can store sperm indefinitely.
Studies have shown that using long-term frozen sperm for assisted reproductive techniques can yield successful outcomes. The success rates of using frozen sperm to achieve pregnancy are comparable to those of using fresh sperm. These rates indicate that frozen sperm can remain viable and capable of fertilization even after many years of storage.
Success Rates of Sperm Storage
The success of sperm storage depends on various factors. Sperm quality, the freezing technique used, and the laboratory's performing procedure expertise are a few factors to consider. Overall, the success rates of using frozen sperm for conception are encouraging.
Studies have shown that the survival rate of frozen sperm after thawing is typically high, ranging from 50% to 80%. Once frozen sperm is thawed, a significant portion remains viable and capable of fertilization.
The success rates of using frozen sperm for assisted reproductive techniques, such as IVF or IUI, are also promising. The chances of achieving pregnancy using frozen sperm are comparable to using fresh sperm. Frozen sperm can be just as effective in achieving conception.
Alternatives to Sperm Storage
Alternative sperm storage options are good for individuals who may not be suitable candidates for this procedure. Some of the alternatives to sperm storage include:
- Testicular Tissue Freezing may be an option for Individuals who cannot produce motile sperm. It could also benefit those at risk of losing their fertility due to medical reasons. Testicular tissue freezing involves removing a small piece of testicular tissue and freezing it for future use.
- Donor sperm is an excellent option for anyone experiencing fertility issues or same-sex couples wanting to start a family. Sperm banks have a collection of donors to choose from. The best part is they're all carefully screened and selected based on the sperm bank's standards. Donor sperm is used in home insemination, intrauterine insemination (IUI), intracervical insemination (ICI), intracytoplasmic sperm injection (ICSI), or in-vitro fertilization (IVF) procedures.
- Adoption can be an excellent option for starting a family. Individuals who cannot conceive naturally or prefer not to pursue assisted reproductive techniques can explore this. Adoption allows individuals to provide a loving home to a child in need.
Individuals must discuss their options with a fertility specialist to determine the most suitable method for preserving their fertility.
The Cost of Sperm Storage
The cost of sperm storage can vary depending on several factors. The cryobank's location, services included, and any additional procedures or tests required to determine the final cost. Sperm storage can range from $500 to $1,500, excluding extra storage or future use fees.
Cryobank America stores sperm for a one-time collection fee of $225 and a monthly storage fee of $18.99. You'll pay a one-time withdrawal fee of $399 when you are ready to use your sample.
Most insurance companies don't cover sperm storage. However, some insurance plans may cover individuals with medical conditions that affect their fertility, such as cancer. Cryobank America has partnered with LIVESTRONG Fertility, offering discounted storage services for registered patients.
Frozen Sperm For Future Fertility
Sperm storage is a valuable option for individuals who wish to preserve their fertility for future use. By freezing and storing their sperm, individuals can maintain their reproductive choices and increase their chances of having future biological children. The process of sperm storage is safe and effective, with high success rates for achieving pregnancy using frozen sperm.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Consider Yoga Before Donating Sperm
Yoga is a practice that has been around for thousands of years and provides numerous benefits for the mind, body, and soul. In recent years, there has been a growing interest in using yoga to improve male fertility, particularly in the context of sperm donation for at-home insemination. This article will explore the concept of Namaste and Conceive, which is the idea of using yoga to improve sperm quality and quantity for successful insemination.
Understanding the Importance of Sperm Quality Before Donating
Sperm quality plays a crucial role in successful insemination. Poor sperm quality can lead to infertility and can also affect pregnancy outcomes. That's why we won't accept sperm samples that fail to meet our criteria. Sperm count, motility, and morphology determine sperm quality. Low sperm count means that there are fewer sperm available for fertilization, while poor motility means the sperm cannot swim effectively toward the egg. Abnormal morphology refers to the shape and size of the sperm, which can also affect their ability to fertilize the egg.

How Yoga Can Improve Sperm Quality and Quantity
Research has shown that yoga can improve male fertility by improving sperm count, motility, and morphology. Yoga helps reduce stress, a significant factor that can negatively impact male fertility. Stress can affect the production of testosterone, which is essential for sperm production. Yoga also helps to improve blood flow to the reproductive organs, which can increase the production of healthy sperm.
The Role of Stress in Fertility and How Yoga Can Help
Stress is a physiological response to a perceived threat or challenge. It triggers the release of hormones like cortisol and adrenaline, which prepare the body for fight or flight. While this response is helpful in short-term situations, chronic stress can negatively affect health.
Chronic stress can also lead to oxidative stress, which can damage sperm DNA and reduce fertility. By reducing stress through yoga, you're on your way to improving the vitality of your sperm and enhancing fertility.
Yoga Poses and Techniques for Improving Sperm Health Before You Donate
Several yoga poses and techniques can improve sperm health. Some of the most effective poses include the Cobra pose, the Bridge pose, and the Shoulder stand. These poses help to improve blood flow to the reproductive organs, which can increase the production of healthy sperm. Other techniques that can help to improve sperm health include deep breathing exercises, meditation, and visualization.
Tips for Incorporating Yoga into Your Routine Before Donating Sperm
Incorporating yoga into your routine before you donate sperm can greatly improve sperm health and increase the chances of successful insemination when a family or individual purchases your vial. Some practical tips for incorporating yoga into your routine include finding a routine that works for you! We all have busy schedules, but once you begin to take steps toward incorporating a yoga routine, it'll become second nature. To start, try practicing consistently and set aside time each day for yoga practice. Setting the alarm for the times you wish to practice each day will ensure you will remember. It is also essential to listen to your body and avoid overexertion. Drink plenty of water so you're staying hydrated.
Lastly, don't give up on trying to enhance your sperm quality with yoga and other meditation practices! At Cryobank America, we're looking for suitable candidates to donate sperm. When you join our program, you can help a family fulfill their dreams of conceiving while you receive extra income!
Click here for more helpful tips.
Click here to learn about our qualifications and incentives for becoming a donor.
It’s often asked, is there a supplement that could help increase your fertility? There is, and it’s called Coenzyme-10, or CoQ10 for short. This supplement is a natural antioxidant that helps with the defragmentation of sperm and the aging process of oocytes. Essentially, it is keeping your eggs and sperm at a healthy young age, even as you age every day. It doesn’t reverse the aging problems that occur naturally with aging but can help stabilize it and reduce the fragmentation of your sperm, which slows the aging process.
CoQ10’s primary purpose was to help heart function, but over the years, fertility doctors and specialists have figured out that it helps sperm and Oocytes as well. Additionally, research shows CoQ10 may be beneficial for Parkinson’s disease patients, can decrease the frequency of migraine headaches, and can enhance energy production to aid in physical performance. You can pick this up over the counter at a local drug store or pharmacies like CVS, Walgreens, or Walmart. It’s relatively inexpensive and could help you and your partner conceive faster! While CoQ10 is considered safe, you should consult your healthcare provider first with all supplements.
If you are wondering about your fertility and want to learn more about your sperm count, you can find more information HERE on how Cryobank America can help!
Have you ever wondered how Cryobanks, Sperm/Egg/Embryo Storage Centers, and Fertility Clinics can store cells that can live for 30+ years? Cryopreservation is the answer, and we want to inform you how we do this.
We use Liquid Nitrogen (LN2) to preserve human cells and tissues in suspended animation at cryogenic temperatures. Liquid Nitrogen is very cold; it is -196 degrees Celsius, or for people in the US, it translates to -321 degrees Fahrenheit. Liquid Nitrogen boils at room temperature, so we must be careful to keep it cold so that it does not boil and get too warm, allowing the cells to thaw out. With the help of freezing media and a proper technique, it will protect the cells from ice crystals, exploding and shrinking.
Doing this results in a preserved cell with an indefinite shelf-life. Once correctly thawed, the cells can resume back to their initial state. Cryopreservation allows people to utilize sperm/eggs/oocytes for future use if they become infertile, which can help many people!
If you would like more information about preserving your ability to conceive in the future, please visit our Directed Donor or Personal Sperm Banking pages, or contact us by email at [email protected] or by phone at 817-945-8708
Yes, by "boys" we mean your testicles. It’s important to know everyday things you do that could decrease your fertility, even in the cold season. Wearing briefs or tights during a workout, setting a laptop on your lap, taking hot baths or long hot showers can all kill your sperm! The reason behind this is that your testicles self-regulate their temperature by having a series of veins called the Pampiniform Plexus surrounding them. In simplified terms, the veins exchange heat, and that will cool the testicles down, but if the area is constantly overheated the Pampiniform Plexus will not work properly.
Another mechanism the testicles use is the ability to bring them closer or farther away from the body. This also allows it to change the temperature, but again, if they are trapped in tight underwear or overheated this will not help save your sperm. If for some reason your sperm count is low, you can try one or all things we have suggested, and in about 60 days you should see an increase in sperm production! Yes, 60 days is a long time, but that is the amount of time it takes to completely cycle through and produce new sperm.
If you are concerned or just generally interested to know how viable your sperm is, please contact us at [email protected] or by phone at 817-945-8708. At Cryobank America, we offer both basic and complete sperm analysis where you can learn about the concentration, motility, vitality, progression, and morphology of your specimen!
ARLINGTON, Texas., September 1, 2017
Cryobank America, the newest sperm bank in the U.S., is pleased to announce its opening in the Dallas-Fort Worth area of Texas.
Located at 3050 S Center St., Suite 100, Arlington, TX 76014, Cryobank America is headquartered in the Medical City District of Arlington between I-20 and I-30 near the University of Texas – Arlington.
With the global sperm shortage causing a previously unseen crisis, many couples and single women are turning to sperm donors to start or expand their families. Dr. Sunday Crider, Ph.D. HCLD/ELD, the Tissue Bank Director and Laboratory Director at Cryobank America, adds, “A simple search online about male infertility and donor sperm shortage yields thousands of results from countries around the world, all facing this same significant issue.”
With the Dallas-Fort Worth area comprising many ethnicities and backgrounds, Cryobank America carefully chose this location amongst many others. “The city of Arlington is in-between two major metropolitan areas in Texas,” Sanjay Kumar, CEO, and Co-founder, explained, “This allows us to choose the best Texans to be a part of our program”.
Rigorous eligibility requirements at Cryobank America ensure that the donors who enter the Sperm Donor Program are narrowed down to only the best candidates. Less than 1% of potential donor applicants become fully eligible donors. Once specimens are moved out of quarantine per FDA requirements, units are shipped worldwide to aid in combating the shortage.
Cryobank America also caters toward directed sperm donors. These donors are men who are either storing their specimen as an insurance policy, should they lose their ability to be fertile in the future, or donors who will be donating their specimen to an intended recipient. “Men in occupations that place them at risk are encouraged to bank their sperm to preserve their fertility, including policemen, firefighters, and military members,” says Dr. Crider. “Additionally, men facing serious illnesses such as cancer or men wanting to get a vasectomy can all benefit from cryogenic preservation of their specimens.”
The staff at Cryobank America comprises highly educated and trained professionals, all holding at least a master’s degree in the biological sciences field. The entire staff is very excited to begin working on helping countless couples and individuals worldwide make their dreams of starting a family a reality.
For more information, contact [email protected]

