When it comes to cryobanking, finding the best California cryobank is crucial. California is home to numerous cryobanks that offer an extensive range of services and options for individuals and couples looking to preserve their fertility or start a family using donor sperm. Choosing the right cryobank is essential to ensure optimal quality of services and the best chance of success in achieving your reproductive goals.
There Are Various California Cryobank Options For Donor Sperm
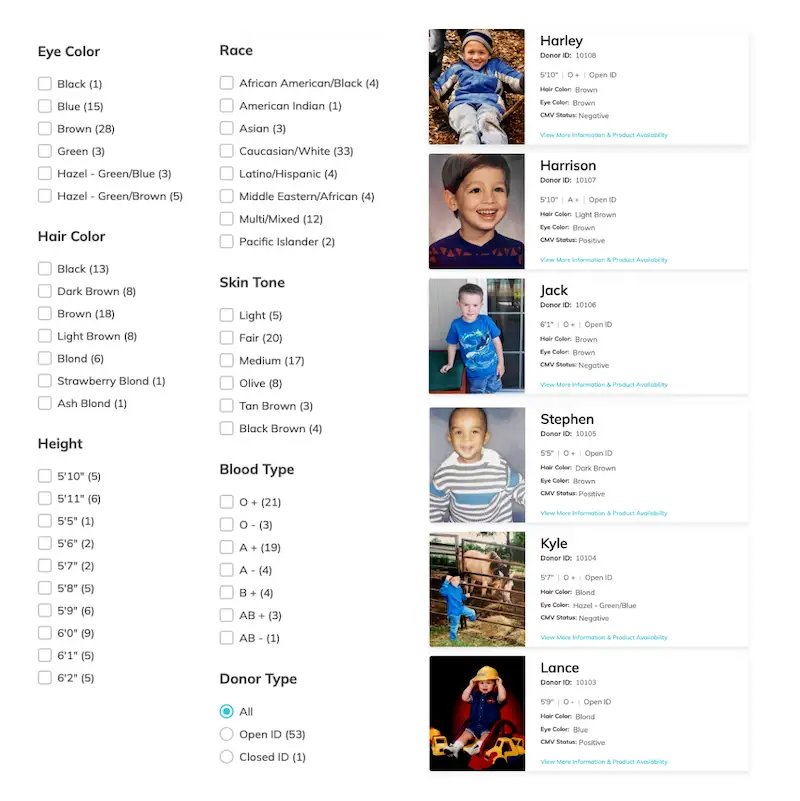
In California, there are various options available when it comes to choosing donor sperm. These options include anonymous donors, known donors, and open donors. Anonymous donors are individuals who choose to remain anonymous and do not have any contact with the recipient or resulting child. Known donors are individuals known to the recipient and may have an ongoing relationship with them. Open donors are individuals willing to have some level of contact with the recipient or resulting child, either through letters, emails, or even in-person meetings.
Choosing the right donor sperm is important based on your preferences and needs. When selecting a donor, it is crucial to consider physical characteristics, medical history, and personal values. Many cryobanks provide detailed profiles of their donors, including information about their physical appearance, education, hobbies, and medical history. Some California cryobanks also offer the option to choose a donor who closely matches your own ethnic or cultural background.
Do I Need To Purchase Donor Sperm From A California Cryobank If I Live In CA?
If you're a California resident, you do not need to purchase donor sperm from a California Cryobank. Many cryobanks around the world deliver donor sperm wherever you reside. Cryobank America offers easy online navigation of donor profiles and vial delivery worldwide.
Understanding the Different Types of California Cryobanks
Different types of cryobanks are available in California, including private and public ones. Private cryobanks are typically for-profit organizations that offer a wide range of services, including egg and sperm storage and donor sperm and egg services. These cryobanks often have many donors and may provide additional services such as genetic testing and counseling.
Public cryobanks, on the other hand, are typically non-profit organizations that focus on providing donor sperm and egg services to individuals and couples who may not be able to afford the high costs associated with private cryobanks. These cryobanks often have a smaller selection of donors and may have stricter recipient eligibility criteria.
Factors to Consider When Choosing A California Cryobank
When choosing a cryobank in California, you should consider several factors. One of the most important factors to consider is the reputation and experience of the cryobank. Choose a cryobank with a good reputation for providing high-quality services to ensure that you receive the best possible care and that the cryopreserved samples are of the highest quality.
Additionally, consider the policies and procedures of the cryobank. These criteria include their donor screening process, quality control measures for cryopreserved samples, and policies regarding releasing information to donors and recipients. Choosing a cryobank with strict policies and procedures ensures the safety of all parties involved.
The Importance of Accreditation and Certification in Cryobanking
Accreditation and certification are important factors when choosing a California Cryobank. Accreditation is a process in which an independent organization evaluates and certifies that a cryobank meets specific standards of quality and safety. Certification, on the other hand, is a process in which a professional organization recognizes a cryobank as meeting particular standards of practice. Cryobank America is fully licensed and registered with the state of California by the State of California Department of Public Health.
Choosing an accredited and certified cryobank can provide reassurance that the cryobank has undergone rigorous evaluation and meets only the highest safety and quality requirements. It can also provide peace of mind knowing that the cryobank is committed to providing its clients the best possible care and services.
How to Evaluate the Quality of Cryopreserved Samples
Evaluating the quality of cryopreserved samples is an essential step in the cryobanking process. The quality of cryopreserved samples can impact the success rates of artificial insemination and reproductive technologies.
There are several factors to consider when evaluating the quality of cryopreserved samples. One factor is the post-thaw survival rate, which refers to the percentage of cells or embryos that survive thawing. A high post-thaw survival rate indicates that the cryopreserved samples have been properly stored and handled and are likely to have a higher chance of success.
Another factor to consider is the viability of the cryopreserved samples. Viability refers to the ability of the cells or embryos to develop and grow after thawing. Choosing a cryobank with high viability rates is essential, as this can increase the chances of a successful pregnancy. Cryobank America conducts a pre and post-thaw count before and after each vial is stored and prepared for delivery. This report is included in your at-home insemination kit to ensure you know the post-thaw results of your donor sperm.
The Role of Donor Screening and Testing in Cryobanking
Donor screening and testing play a crucial role in the cryobanking process. Donor screening evaluates potential donors to ensure they meet specific criteria, such as being free from infectious diseases and having a healthy medical history. On the other hand, donor testing involves conducting various tests on the donor's biological samples to ensure they are free from genetic disorders or other hereditary conditions.
Cryobanks in California may perform different types of donor screening and testing. These may include infectious disease testing such as HIV, hepatitis B and C, syphilis, and cytomegalovirus (CMV). Donor testing may also include genetic screening for conditions like cystic fibrosis, sickle cell disease, and thalassemia.
Choosing A California Cryobank
Choosing a California cryobank with strict donor screening and testing protocols is essential to ensure the safety of the donor and the recipient. These standards can minimize the risk of transmitting infectious diseases or genetic disorders.
Finding The Highest Quality Donor Sperm in California
Finding the highest quality donor sperm in California requires careful consideration and research. Choose a reputable cryobank that has a track record of providing high-quality donor sperm and has strict quality control measures in place.
One way to find the highest quality donor sperm is to choose a cryobank that offers comprehensive genetic testing for donors. Testing can assist in identifying any potential genetic disorders or hereditary conditions that may be present in the donor's genetic makeup. Expanding your search and looking into cryobanks outside of California is essential, as this can increase the chances of finding a donor who closely matches your preferences and needs.
Cost and Payment Options for California Cryobank Services
The cost of cryobanking services in California can vary depending on the cryobank and the specific services provided. Consider the cost of cryobanking when deciding, as it can be a significant financial investment.
In addition to the cost of cryobanking, consider the available payment options. Some cryobanks may offer financing options or payment plans to make costs more manageable. Cryobank America provides affordable pricing and financing options, making donor sperm more accessible to everyone. Check with your insurance provider to see if your insurance plan covers services provided by California cryobanks before you start your donor search.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
The Primary Components of Sperm
Sperm is a fluid that results from ejaculation from the penis during sexual intercourse. It is composed of various components, each serving a specific function. Learn about the details of sperm, what each element consists of, and their essential functions.
Secretion From The Cowper's Glands
The secretion from the Cowper's glands, also known as bulbourethral glands, is a clear, viscous fluid. It contains mucus and various enzymes, such as prostate-specific antigen (PSA), which helps to neutralize the acidity of the urethra and lubricate the passage for sperm during ejaculation.
Other enzymes in this secretion include:
1. Mucin: It is a glycoprotein that helps in lubricating the urethra and facilitates the passage of semen during ejaculation.
2. Proteolytic enzymes: These enzymes help in breaking down proteins present in the semen, which aids in liquefaction of the ejaculate.
3. Acid phosphatase: It is an enzyme that helps in maintaining the acidic pH of the semen, which is vital for sperm function and survival.
4. Fibrinolysin: This enzyme helps break down fibrin, a protein involved in blood clotting. Its presence in the Cowper's gland secretion helps to prevent the clotting of semen within the urethra.
These enzymes collectively contribute to the composition and function of the Cowper's gland secretion during sexual arousal and ejaculation.
PSA (Prostate-Specific Antigen) In Sperm
PSA (Prostate-Specific Antigen) is an enzyme that helps to liquefy sperm, allowing it to become more fluid and mobile. Liquefaction plays a crucial role in facilitating the mobility and viability of sperm cells as they navigate through the female reproductive system.
PSA is tested to check for prostate cancer because it is a protein produced by the cells of the prostate gland. Elevated levels of PSA in the bloodstream may suggest the existence of prostate cancer or other prostate-related ailments, such as prostatitis or benign prostatic hyperplasia (BPH). However, it is essential to note that an elevated PSA level does not necessarily mean a person has prostate cancer, as other factors can also cause PSA levels to rise. Therefore, PSA testing serves as an initial screening tool to identify whether an individual needs further evaluation for prostate cancer.
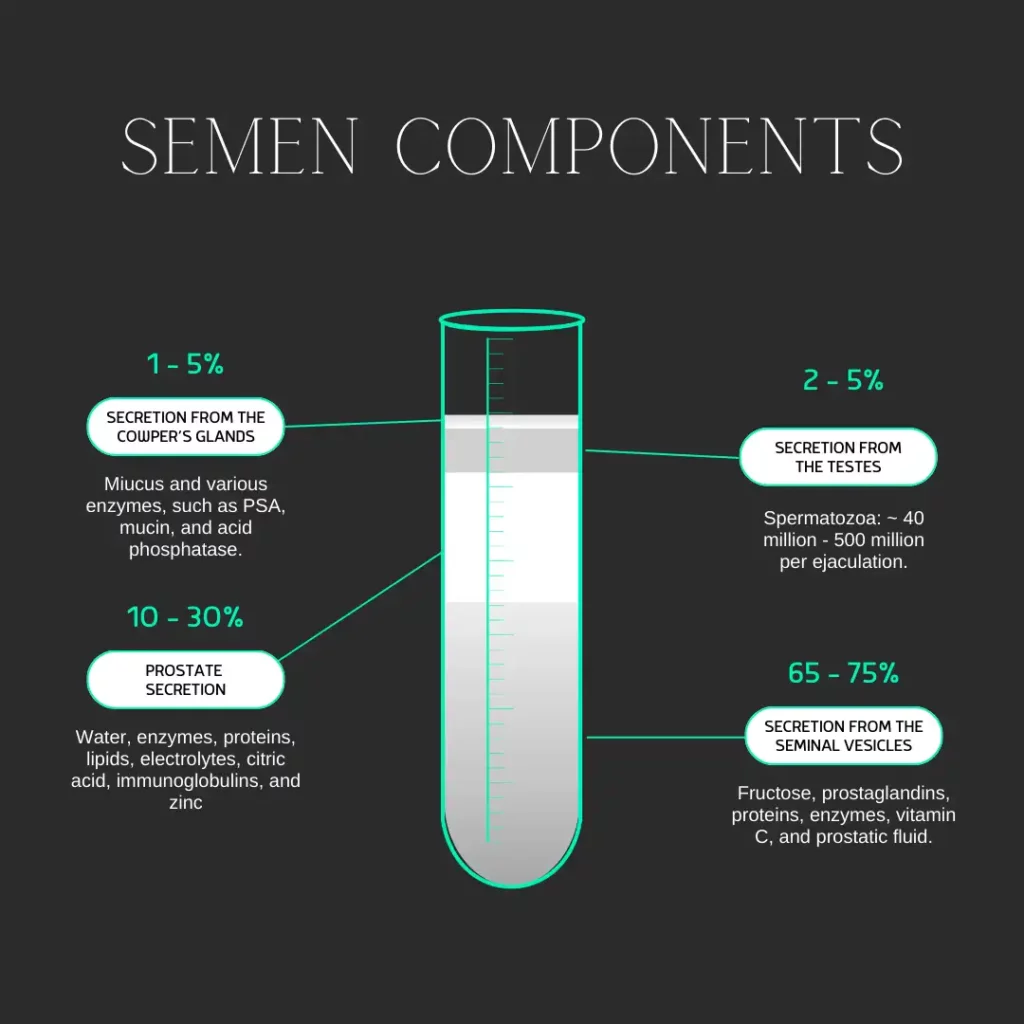
Secretion From The Testes
The secretion from the testes primarily consists of sperm cells and various hormones, including testosterone, dihydrotestosterone (DHT), and inhibin.
Spermatozoa (Sperm Cells)
Spermatozoa, also known as sperm cells, are the reproductive cells produced in the testes. They are responsible for fertilizing the female egg during sexual reproduction. The number of sperm cells produced in the testes and released during one ejaculation can vary. The testes produce around 100 million to 300 million sperm cells daily. However, during ejaculation, the number of sperm cells released is typically much lower.
A typical ejaculation can release anywhere from 40 million to 500 million sperm cells. Some ejaculates may contain more than a billion cells. The number can depend on overall health, age, and sexual activity.
Testosterone In Sperm
Testosterone, the primary male sex hormone, is secreted from the testes. It plays a pivotal role in maintaining and producing male reproductive tissues and secondary sexual characteristics. Testosterone stimulates the growth and development of the male reproductive organs, including the testes, prostate gland, and seminal vesicles. It also promotes the production of sperm cells in the testes.
Apart from its crucial role in male reproductive function, testosterone also impacts a range of other physiological processes in males. It helps regulate muscle mass and strength, bone density, and red blood cell production. Testosterone is also involved in maintaining libido (sex drive) and regulating mood and cognitive function.
Overall, testosterone is essential for the proper functioning of male reproductive organs and has a significant impact on various aspects of male physiology and behavior.
DHT
Dihydrotestosterone (DHT) is a hormone predominantly synthesized in the testes and plays a pivotal role in the establishment and sustenance of male sexual traits. DHT is accountable for the growth and maturation of the male reproductive system, encompassing the penis, scrotum, and prostate gland. Furthermore, it aids in developing secondary sexual characteristics, such as facial and body hair growth, muscle mass, and deepening of the voice. Moreover, DHT is instrumental in regulating libido and contributes to sperm production.
Inhibin
Inhibin is a hormone secreted by the Sertoli cells in the testes. It plays a role in the negative feedback regulation of the hypothalamic-pituitary-gonadal axis (a complex hormonal system that regulates reproductive function in both males and females). Inhibin inhibits the secretion of follicle-stimulating hormone (FSH) from the anterior pituitary gland. By suppressing FSH secretion, inhibin helps regulate spermatogenesis and maintain optimal testosterone levels in the testes.
Prostate Secretion In Sperm
Prostate secretion is composed of several components, including:
1. Water: Most prostate secretions are water, which helps dilute and transport other components.
2. Enzymes: The prostate gland produces several enzymes, including prostate-specific antigen (PSA), which helps to liquefy semen after ejaculation.
3. Proteins: Prostate secretion contains various proteins, such as prostate-specific acid phosphatase (PSAP) and prostate-specific membrane antigen (PSMA), which regulate cell growth and function.
4. Lipids: Prostate secretion contains lipids, including cholesterol and fatty acids, which help to maintain the integrity of the cell membranes and provide energy.
5. Electrolytes: The prostate gland secretes a variety of electrolytes, including sodium, potassium, calcium, and magnesium, that play a crucial role in regulating fluid balance within the body.
6. Citric acid: The prostate gland produces citric acid, which helps to provide energy for sperm motility.
7. Zinc: Prostate secretion contains high levels of zinc, which is important for maintaining prostate health and function.
8. Immunoglobulins: Prostate secretion contains immunoglobulins, such as IgA and IgG, which help to protect against infections and maintain immune function in the reproductive system.
Each component works together to nourish and protect sperm cells during ejaculation.
Secretion From The Seminal Vesicles
The seminal vesicles, located behind the bladder in males, are a vital pair of small glands that play a crucial role in producing semen. This fluid serves as a carrier for sperm during ejaculation. The components of seminal vesicles in semen include:
1. Fructose: Seminal vesicles produce fructose, a type of sugar that provides energy for sperm cells.
2. Prostaglandins: These are hormone-like substances that help in the contraction of the female reproductive tract, aiding in sperm movement towards the egg.
3. Proteins and enzymes: Seminal vesicles secrete various proteins and enzymes, including fibrinogen, prostate-specific antigen (PSA), and different proteolytic enzymes. These substances help in the coagulation and liquefaction of semen.
4. Vitamin C: Seminal vesicles also contribute vitamin C to semen, which helps protect sperm cells from oxidative damage.
5. Prostatic fluid: While not directly produced by the seminal vesicles, prostatic fluid is often mixed with seminal vesicle secretions to form semen. The prostatic fluid contains enzymes, citric acid, zinc, and other substances that nourish and protect sperm cells.
Overall, the components produced by seminal vesicles play crucial roles in providing energy to sperm cells, aiding their movement through the female reproductive tract, and protecting them from oxidative damage.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
The Pivotal Role of Hydration in Fertility
Fertility, a crucial aspect of human health and well-being, is intricately linked to one's overall physical condition. A couple of factors contribute to fertility, with general health being at the forefront. Among these, hydration stands out as a fundamental yet often overlooked element. Just as reducing harmful habits like smoking and alcohol consumption, along with maintaining a balanced exercise regimen, is essential for reproductive health, so is ensuring adequate hydration. This article delves into the pivotal role of hydration in fertility, exploring its impacts and distinguishing its importance from other lifestyle factors.
The Importance of Hydration for Fertility
Hydration plays a critical role in fertility, more than what might be immediately apparent. The human body, a complex system reliant on water for all its functions, sees its reproductive capabilities significantly influenced by hydration levels. For both men and women, adequate hydration is essential for maintaining optimal reproductive health.

Hormonal Balance and Ovulation
In women, hydration is crucial for the hormonal balance necessary for regular menstrual cycles and ovulation. The body's ability to produce cervical fluid, vital for helping sperm reach the egg, is also heavily dependent on hydration. Dehydration can compromise egg health, leading to reduced fertility. On the other hand, a well-hydrated body ensures that the reproductive system functions at its best, setting a conducive environment for conception.
Sperm Count, Production, and Quality
For men, hydration is equally important. Sperm production and quality are sensitive to the body's hydration levels. Dehydration can lead to a lower sperm count and reduced semen volume, both of which are key factors in male fertility. Proper hydration ensures that the sperm are healthy and viable, increasing the chances of successful conception.
Other Factors
Hydration's role in fertility is distinct from other lifestyle factors like diet, exercise, or the avoidance of harmful substances. While all these elements contribute to overall health and by extension, fertility, hydration directly affects the body's ability to reproduce at a cellular level. It is a fundamental requirement for the proper functioning of the reproductive organs and the hormonal systems that regulate them.
Unlike other lifestyle changes that might take time to impact fertility, the effects of hydration or dehydration are more immediate and direct. Thus, while it is part of a broader spectrum of health behaviors conducive to fertility, hydration deserves special attention due to its immediate and profound impact on reproductive health.
Sources of Hydration Beyond Water
While water is the most direct source of hydration, there are other effective alternatives. Flavor-enhanced water, such as those with added natural fruit essences or electrolytes, can be more appealing and encourage regular fluid intake. These options can make staying hydrated an enjoyable part of your day. Additionally, incorporating water-rich fruits and vegetables into your diet is an excellent strategy. Foods like cucumbers, tomatoes, watermelons, and oranges are not only high in water content but also provide essential vitamins and minerals. These natural sources of hydration can be particularly beneficial for those who struggle with drinking enough plain water.
Hydration as Part of a Fertility-Boosting Diet
Hydration is a key factor in a diet aimed at boosting fertility. A well-rounded nutritional plan that includes sufficient fluid intake is crucial for optimal reproductive health. Hydrating foods, particularly fruits and vegetables, offer the dual benefits of hydration and essential nutrients. For example, leafy greens and berries are rich in antioxidants and vitamins that are vital for fertility. Additionally, these water-rich foods help in the absorption of other important nutrients and contribute to the overall balance of the diet. Integrating hydration into your dietary regimen ensures that both solid and liquid nutritional needs are met, creating a conducive environment for fertility.
Practical Tips for Maintaining Optimal Hydration
Staying well-hydrated is essential for overall health and fertility, and there are practical ways to ensure you meet your hydration needs. Firstly, aim to consume the recommended daily water intake, which varies based on factors like age, gender, climate, and activity level. Including a variety of hydrating foods in your diet, such as fruits and vegetables, can also contribute to your overall fluid intake. Pay attention to the color of your urine as an indicator of hydration; a light, straw color suggests adequate hydration, while a darker color may indicate a need for more fluids. Additionally, carrying a water bottle throughout the day can serve as a constant reminder to drink water regularly. Simple lifestyle adjustments like these can make a significant difference in maintaining optimal hydration levels.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
The Vital Role of Diet in Enhancing Fertility: Understanding Nutritional Impacts
Fertility, a vital aspect of human health, is profoundly influenced by various factors, among which diet plays a crucial role. This article delves into the significant impact of nutrition on reproductive health, exploring how various nutrients contribute to enhancing fertility in both men and women.
Understanding Fertility and Nutrition
Fertility, the ability to conceive a child, is a complex interplay of various biological processes in both genders. In women, it involves the production of viable eggs, regular menstrual cycles, and a conducive uterine environment for embryo implantation. For men, it centers around the production of healthy sperm with adequate motility and count. The role of nutrition in this context is pivotal.
A well-balanced diet not only supports the normal functioning of reproductive systems but also improves the overall chances of conception. Diet influences hormonal balance, ovulatory function, and sperm quality, thereby directly impacting fertility.
Key Nutrients and Their Impact on Fertility
How Folic Acid Can Help
Paramount in the realm of reproductive health is folic acid, a B vitamin essential for cellular growth and reproduction. Its significance cannot be overstated, particularly in preventing neural tube defects in the developing fetus, such as spina bifida and anencephaly. For women trying to conceive, an adequate intake of folic acid enhances the chances of a healthy pregnancy. Foods rich in folic acid include leafy greens, legumes, and fortified cereals.
Omega-3s and Antioxidants
These nutrients play a vital role in maintaining the quality of eggs and sperm. Omega-3 fatty acids, found in fish, seeds, and nuts, are crucial for hormonal function and may improve sperm motility. Antioxidants, like vitamins C and E, protect reproductive cells from oxidative stress, enhancing their quality and lifespan. These nutrients are abundant in fruits, vegetables, and whole grains.
B Vitamins
Beyond folic acid, other B vitamins also contribute significantly to fertility. For instance, vitamin B12 is vital for the proper functioning of the nervous system and the production of DNA, both essential for a healthy pregnancy.
Macronutrients Balance
The right balance of proteins, carbohydrates, and fats is essential for optimal fertility. High-quality proteins from plant sources, such as legumes and nuts, are associated with improved fertility compared to proteins from red and processed meats. Complex carbohydrates found in whole grains stabilize blood sugar and insulin levels, which is crucial for hormonal balance. Healthy fats, especially unsaturated fats, support reproductive hormone production. Conversely, trans fats, often found in processed foods, should be avoided as they negatively impact ovulation.
Diet and Its Direct Influence on Reproductive Disorders
Diet significantly influences reproductive disorders, affecting menstrual cycle regularity and spermatogenesis. Nutritional deficiencies or excesses can lead to menstrual irregularities, impacting ovulation and overall fertility. Similarly, spermatogenesis, the process of sperm production, relies on specific nutrients for optimal function. Conditions like endometriosis, characterized by painful periods, and dysmenorrhea, severe menstrual cramps, can also be influenced by dietary factors. For instance, diets high in processed foods and low in essential nutrients can exacerbate these conditions, whereas a balanced diet can help manage symptoms and improve reproductive health.
Are Processed Foods Really That Bad For Fertility?
According to a Harvard study, consuming beverages high in sugar was linked to a decrease in fertility for both men and women, however, drinking diet sodas and fruit juices seemed to have no effect. The study also showed that women who consumed high quantities of fast food took longer to become pregnant compared to women who skipped fast food and consumed more fruits and veggies. Additionally, It found that couples who consumed sufficient amounts of seafood were likely to get pregnant sooner.
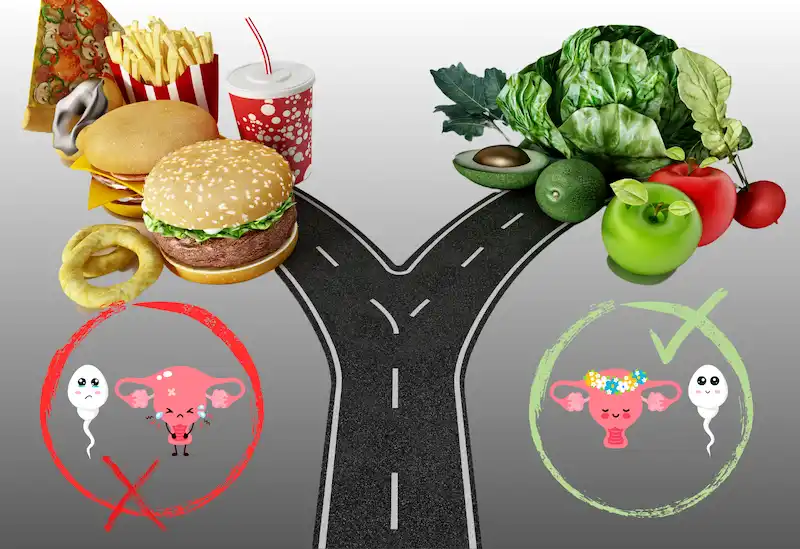
There are many reasons processed food has a negative effect on fertility. As previously mentioned, processed foods are often stripped of their natural nutrients during the manufacturing process. This can lead to deficiencies in essential vitamins and minerals that are important for reproductive health, such as folate, iron, and zinc. Many processed foods contain artificial additives, preservatives, and chemicals that can disrupt hormonal balance in the body. Hormonal imbalances can interfere with ovulation and sperm production, making it more difficult to conceive. They're also typically high in refined carbohydrates, unhealthy fats, and added sugars. These ingredients can promote inflammation in the body, which has been linked to infertility in both men and women. Processed foods are often calorie-dense but nutrient-poor, leading to weight gain and obesity. Excess weight can negatively impact fertility by disrupting hormone levels and interfering with ovulation. This can lead to an increased risk of conditions that can affect fertility, such as polycystic ovary syndrome (PCOS) and endometriosis.
Practical Dietary Recommendations for Enhancing Fertility
To enhance fertility, focusing on a diet rich in plant-based proteins and reducing processed food intake is essential. Plant-based proteins like legumes, nuts, and seeds provide essential nutrients without the adverse effects associated with processed meats. Achieving and maintaining a healthy weight is crucial, as weight extremes can disrupt hormone balance and ovulation. A diet inclusive of whole grains, fruits, vegetables, and lean proteins can support a healthy weight and improve fertility. Additionally, incorporating foods rich in antioxidants, vitamins, and minerals can enhance reproductive health. For those trying to conceive, a well-balanced, nutrient-rich diet is a key step towards fertility success. Learn which 6 foods have been proven to boost fertility.
Limitations and Other Considerations
While diet plays a crucial role in fertility, it's important to acknowledge that it's not a cure-all for fertility issues. Factors like age, genetic predispositions, and underlying medical conditions also significantly impact fertility. A healthy diet can support reproductive health, but it's one aspect of a multifaceted approach to addressing fertility challenges. Therefore, alongside dietary changes, consulting healthcare professionals for a comprehensive fertility assessment is crucial.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Choosing IUI, ICSI, or At-Home Insemination Over IVF: 4 Factors You Should Know
Exploring different fertility treatment options requires a deep understanding of various factors, ranging from medical to financial, to personal preferences. While In-Vitro Fertilization (IVF) is undoubtedly one of the most recognized fertility treatments, other methods like Intrauterine Insemination (IUI), Intracytoplasmic Sperm Injection (ICSI), and at-home insemination have their unique appeal and benefits. But what drives the decision to choose one over the other? Here, we delve into the reasons.
1. Choosing IVF For Fertility Health and Specific Challenges
The first and foremost consideration is the specific fertility challenge a couple or individual is facing. While IVF is robust and addresses a wide array of fertility issues, some challenges may be addressed more directly with other treatments.
Male Infertility Issues
ICSI, a specialized form of IVF, has emerged as a game-changer for couples dealing with male infertility. By directly injecting a single healthy sperm into an egg, it bypasses challenges like low sperm count or poor sperm mobility. Thus, for those who have identified male infertility as the primary obstacle, ICSI might be a more direct solution than traditional IVF.
Uncomplicated Infertility Or Use Of Donor Sperm
For women with open fallopian tubes, regular ovulation, and no apparent severe infertility issues, IUI provides a less invasive approach. It's particularly popular among single women or lesbian couples using donor sperm.
2. Choosing IUI Or At-Home Insemination Due To Financial Considerations
Fertility treatments can be expensive, and not everyone has the luxury of unlimited resources or comprehensive insurance coverage.
Which Procedure Is Less Expensive, IUI or IVF?
Generally, IUI is less expensive than IVF or ICSI. For those who are on a tighter budget, starting with IUI might be a feasible first step. If several IUI cycles don't result in pregnancy, they might then consider investing in IVF or ICSI.
Cumulative Costs — What's Really More Expensive, IUI or IVF?
It's also essential to consider cumulative costs. While IUI per cycle might be cheaper, if multiple cycles are needed, the costs can add up. In contrast, IVF, though pricier upfront, might offer a higher success rate per cycle. The bottom line will be determined by your overall fertility health, donor or partner compatibility, and timing insemination correctly by precisely tracking your ovulation cycle.
Many cryobanks offer financial services such as payment plans and financing. Cryobank America has partnered with Future Family to offer patients affordable financing options.

3. Choosing IUI, IVF, or At-Home Insemination For Personal Preferences and Comfort
Medical procedures, even if they're routine from a clinical perspective, are deeply personal experiences.
Invasiveness and Comfort — IUI
IUI stands distinct with its simplicity. By directly introducing sperm into the uterus, it bypasses many of the steps intrinsic to IVF, such as egg retrieval and external fertilization. This straightforwardness can be less daunting for those who are apprehensive about medical procedures. The very nature of IUI, being less invasive, can also mean reduced physical discomfort, fewer side effects, and a shorter recovery period.
For many, starting with IUI is a gentle introduction to fertility treatments. The rationale often revolves around giving the less invasive method a try first, hoping it might lead to successful conception without the need for more complex procedures.
Natural Conception
Fertility treatments, for all their medical advancements, can sometimes feel clinical and detached from the intimate experience of conception. This feeling can be a significant determinant in the choices couples make. There's an inherent appeal in procedures that mimic or come close to the process of natural conception.
IUI, especially when executed without the aid of fertility drugs, offers an experience that's remarkably close to natural conception. The process aligns with the body's natural ovulation cycle, and the sperm is introduced directly into the uterus without any external fertilization. This method provides couples with a sense of familiarity and naturalness, making the journey feel less 'medical' and more intimate.
At-Home Insemination
The appeal of at-home insemination lies in its intimacy and privacy. For those who find clinical settings stressful or impersonal, at-home insemination offers a more comfortable and familiar environment. This method is also more cost-effective than clinical procedures, though it may have a lower success rate and lacks the oversight and expertise of a medical setting.
4. Treatment Duration and Timelines
For some, the time it takes from starting treatment to achieving pregnancy is a significant factor.
Which Procedure Is Quicker, IUI or IVF?
IUI stands out as a relatively quicker procedure when juxtaposed against IVF (in vitro fertilization). The simplicity of IUI, which involves directly introducing sperm into the uterus, eliminates several steps intrinsic to the IVF process, such as egg retrieval and lab fertilization. For those already navigating the emotionally charged waters of fertility challenges, the shorter treatment duration of IUI can be a breath of fresh air. It offers hope without the extended commitment, making it an attractive choice for those wary of prolonged medical interventions.
Does IUI or IVF Have A Higher Success Rate?
Time considerations in fertility treatments aren't just about the procedure's speed. It's also about effectiveness across multiple cycles. Here's where the dynamics become intricate. IVF, despite its lengthier process, often touts a higher success rate per cycle when compared to IUI. This statistic can translate to fewer overall treatment cycles, potentially shortening the entire duration from the start of treatment to conception.
On the flip side, the non-invasiveness, simplicity, and lower immediate costs of IUI can lead some to opt for multiple IUI cycles before considering the switch to IVF. The thought process here hinges on hope: the hope that the next IUI cycle might be a successful one, coupled with the procedure's relative simplicity.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Comparing IVF, ICSI, and IUI: Understanding Your Options in Fertility Treatments
Embarking on the path to parenthood, many couples and individuals find themselves at the crossroads of fertility treatments. The journey, while filled with hope, often presents a maze of medical terms, techniques, and decisions. The options — IVF, ICSI, and IUI — though different, all aim to assist in the realization of the dream of having a child. Delving deeper into each method helps demystify the process and sheds light on the complications involved.
Please make sure to also contact a suitable health professional. While this article is your information guide, it is not to be used as a substitute for medical opinion or healthcare treatment.
IVF (In-Vitro Fertilization)
IVF involves stimulating the ovaries using fertility drugs to produce mature eggs. These eggs are then retrieved and fertilized in a lab with sperm from a partner or a donor. The resultant embryo is monitored for signs of fertilization, and the best-quality embryo is transferred to the uterus.
Advantages of IVF
IVF is a comprehensive treatment that can address both male and female infertility factors. Through IVF, mature eggs are retrieved and fertilized in a laboratory setting, and the best-quality embryos are chosen for transfer, increasing the chances of success. The process allows for advanced embryo selection techniques, such as time-lapse monitoring and Preimplantation Genetic Screening. This ensures only embryos with the highest potential are selected. IVF provides the flexibility to use either a partner's or a donor's sperm, giving diverse options for family planning. Additionally, if more than one high-quality embryo results from the cycle, the extra embryos can be frozen for future use.
When is IVF advised?
IVF is typically recommended for those with fallopian tube damage, blockages, or in cases of unexplained infertility. It's also a viable option in mild cases of male infertility.
ICSI (Intracytoplasmic Sperm Injection)
ICSI (Intracytoplasmic Sperm Injection), on the other hand, is a refined version of IVF. Instead of allowing sperm to fertilize the egg naturally in a dish, ICSI involves the direct injection of a single, chosen sperm into the egg. This technique proves invaluable, especially in cases where male infertility is a concern. By bypassing many natural challenges, ICSI offers a chance even when sperm count is low or mobility is compromised.

Advantages of ICSI
ICSI is a specialized form of IVF where a single, healthy sperm is injected directly into the egg. This direct approach maximizes the chance of fertilization, especially in cases of male infertility. Since only the best quality sperm is selected and used, it ensures the highest potential for successful fertilization. ICSI is particularly beneficial when there are significant sperm problems, such as a low sperm count, poor sperm mobility, or high levels of DNA damage in the sperm. Even when sperm needs to be surgically retrieved, ICSI can still be applied. By addressing male fertility issues directly, ICSI bypasses many obstacles that can prevent natural fertilization.
When is ICSI advised?
ICSI is commonly prescribed for those with male fertility problems such as low sperm count, poor sperm mobility, or high levels of DNA damage in sperm. If male fertility isn't the primary issue, IVF is usually the suggested method.
IUI (Intrauterine Insemination)
IUI (Intrauterine Insemination) stands apart from the aforementioned methods. It is less invasive and mirrors the process of natural conception more closely. In this procedure, prepared sperm is directly introduced into the uterus, timed with ovulation, to facilitate fertilization. For many, IUI serves as a starting point in their fertility journey, especially when the primary concern is not related to sperm quality or quantity.
Advantages of IUI
IUI is a straightforward, non-invasive procedure without the need for anesthesia. It's generally more affordable than advanced fertility treatments such as IVF or ICSI. The entire IUI process can be completed within minutes, making it a quick and hassle-free option. The sperm "washing" process ensures that only the best and healthiest sperm are used for insemination. The timing of the insemination is carefully synchronized with the woman's ovulation to increase the chances of success. IUI can effectively address a range of infertility issues, from unexplained infertility to mild male factor problems. It's also a preferred method when using donor sperm, offering a simpler path for diverse family planning. Unlike some other treatments, there's no need for egg retrieval or surgical intervention, making it less physically demanding.
When is IUI advised?
IUI is an option for patients requiring donor sperm. To succeed, it requires clear fallopian tubes, a healthy sperm count, and a mature egg. In cases of irregular ovulation, fertility drugs may be combined with IUI.
Which Treatment is Right for You?
Your unique fertility situation will determine the best treatment. A comprehensive assessment considering your medical history, age, and response to previous treatments is necessary. For some, IUI might be the first step. However, if significant sperm disorders are detected, IVF or ICSI might be more suitable.
It's essential to understand that your fertility journey is individual. The goal is to achieve pregnancy in the most efficient and effective manner. Always ensure that you are part of the decision-making process, aware of the costs, and fully informed about the treatment path ahead.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
The Impact of Supplements on Fertility: What You Need to Know About Harmful Supplements for Fertility
In today's health-conscious world, dietary supplements have surged in popularity. While they intend to enhance one's nutritional intake, a disconcerting truth is that some of these over-the-counter remedies can have deleterious effects on fertility. It's imperative that individuals, particularly those seeking to conceive, be aware of the potential risks.
Most individuals presume that supplements, especially those available without a prescription, are safe. This perception couldn't be further from the truth. As Marta Montenegro, a fertility lifestyles specialist, notes, over 70% of Americans consume supplements that might inadvertently impede their fertility. The reason? These are not mere "gummies"; they carry the weight of medicines, influencing metabolism, hormones, and the critical endocrine system governing fertility.
Further, Dr. Daniel A. Skora, a reproductive endocrinologist, stresses that many supplements, even those sold online, are unregulated. Absent any oversight on dosage or efficacy, the risks amplify.
While many supplements are available, let's delve into those that specialists have identified as potential threats to fertility:
For those trying to conceive, understanding how medications and supplements affect fertility is vital. Here's a closer look at 12 potential culprits, their effects, and alternative considerations.
Medications and Supplements that may Impact Fertility
Alpha Blockers - These are frequently prescribed for urinary problems stemming from an enlarged prostate. However, an unforeseen side effect is that they can affect the process of ejaculation, potentially complicating conception.
Testosterone Replacement Therapy - Aimed at addressing low testosterone levels, this treatment might seem beneficial. However, an unintended consequence is a reduced sperm count or even cessation of sperm production altogether.
Depression Medications - Among the myriad side effects of certain antidepressants, some can disrupt male sexual functions, such as ejaculation. For women, they can tamper with the ovulation process and inadvertently influence hormone levels.
Steroids - Anabolic steroids are notorious for interfering with sperm production in men. In women, some types of corticosteroids can impede the release of hormones pivotal for ovulation.
Thyroid Medication - It's a double-edged sword. While they can be beneficial for fertility, if not accurately dosed, they can disturb prolactin levels, subsequently affecting ovulation.
Antiepileptic drugs & Antipsychotics - Both of these medications have been linked to fertility issues. Not to mention, cancer treatments, especially chemotherapy, have profound, lasting effects on fertility in both genders.
Black Cohosh - Despite its popularity for treating menopausal symptoms, it presents a potential risk. If consumed during pregnancy, it can trigger premature labor.
Vitamin A - A crucial vitamin for numerous body functions. But in high concentrations, particularly during early pregnancy stages, it can induce congenital birth anomalies.
Weight Loss Supplements - A majority have stimulants, which can introduce risks for women contemplating pregnancy.
Megavitamins - It's all about balance. Elevated levels of specific nutrients might compromise a pregnancy's success.
Dong Quai - Renowned as the “female ginseng”, it poses a risk by potentially triggering uterine contractions, upping the odds of miscarriage.
Testosterone Boosting Supplements - In females, they can adversely affect the fetus. In males, they can decrease sperm counts.

Supplements Beneficial for Fertility
Supplements Beneficial for Fertility
Prenatal Vitamins - They're packed with folic acid and iron, both vital during a baby’s early developmental stages. Ideally, women planning to conceive should begin these supplements in advance of pregnancy.
Omega 3 Fatty Acids - They play a multifaceted role. They help regulate hormones, improve the uterus's blood flow, and facilitate embryo implantation. If fish isn't a dietary staple, supplements such as fish or algal oil can suffice.
CoQ10 - Known for its antioxidative properties, CoQ10 has shown promise in enhancing ovarian response and boosting conception rates for women undergoing fertility treatments. It's imperative to consult a healthcare professional before introducing it to your regimen.
Vitamin D - A deficiency in this essential vitamin can be an obstacle to conception. While sunlight and seafood are natural sources, supplements can bridge any gaps, but ensure a doctor's guidance on the correct dosage.
Substances like alcohol, marijuana, and tobacco can also negatively impact fertility. For instance, heavy drinking and smoking can lower testosterone and sperm counts in men and hamper female reproductive health.
Important Note:
Self-diagnosis, driven by symptoms we recognize from online descriptions, can be misleading. Our bodies are complex systems, where symptoms can often indicate multiple conditions. Making assumptions based solely on general information can lead us down a path of incorrect self-treatment, which can, at best, be ineffective and, at worst, harmful. For example, taking a supplement believed to boost fertility based on an article or testimonial without understanding its full effects or interactions with other medications can have unforeseen consequences.
When considering conception, the stakes are even higher. Both partners' health plays a critical role in the likelihood of conceiving and ensuring a healthy pregnancy. Making uninformed changes to medication or supplement intake can not only affect the chances of conception but can also impact the health of the fetus. Certain medications, even those perceived as benign or beneficial, can have teratogenic effects, potentially causing congenital anomalies.
Moreover, everyone's body is unique. A medication or supplement that works wonders for one individual might have a neutral or negative effect on another. This variability can be due to genetics, existing health conditions, lifestyle factors, or other medications being taken. Only a healthcare professional with a comprehensive understanding of an individual's medical history and current state can provide advice tailored to that specific person.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
How To Choose The Right Cryobank — Finding A Donor, Becoming A Donor, And Semen Cryopreservation
Assisted reproduction, whether as a donor or a recipient, involves several crucial decisions. It is a noble endeavor through which one can bring happiness into others’ lives. However, making such a decision requires a thoughtful process. One of the most significant is selecting the right cryobank. A cryobank specializes in the collection, analysis, and storage of human sperm, which can be a lifeline for couples struggling with infertility, single women, or LGBTQ+ couples looking to start a family. Here's a comprehensive guide to navigating the process of choosing the right cryobank, understanding semen cryopreservation, and the intricacies of becoming or finding a donor.
Understanding the Role of a Cryobank
When seeking a sperm donor, several factors come into play. You'll want to consider the donor's health history, physical traits, educational background, and even hobbies or personality traits. Reputable cryobanks provide extensive profiles for each donor, which can help match recipients with donors that meet their specific criteria.
- Diversity and Variety - Look for a cryobank with a wide selection of donors from various ethnic backgrounds, physical characteristics, and personal achievements.
- Transparency - Ensure that the cryobank provides comprehensive medical and psychological screening results of their donors.
- Legal Standards - The cryobank should operate under the strict guidelines set by health authorities and government bodies.
Becoming a Donor: What to Expect
If you're considering becoming a sperm donor, it's important to choose a cryobank with clear, ethical guidelines and rigorous health screening processes.
- Screening Process - Be prepared for in-depth health screenings, including blood tests, semen analysis, genetic testing, and psychological evaluations.
- Commitment - Understand the time commitment involved, as the process might require regular donations for a period.
- Anonymity and Discretion - Decide your preference for future contact with any children born from your donations. Some donors prefer to remain anonymous, while others are open to contact.

Semen Cryopreservation: The Science of Sperm Freezing
Semen cryopreservation, or sperm freezing, is a scientific process where sperm cells are preserved at sub-zero temperatures (-196°C). This process ensures the long-term viability of the sperm, maintaining its integrity for future use in assisted reproductive techniques like In Vitro Fertilization (IVF) or Intrauterine Insemination (IUI). If you are opting for this process, consider the following options.
- Ensure the cryobank uses reliable freezing techniques, guaranteeing the sperm's viability for several years.
- Inquire about the cryobank's procedures for storing and handling the sperm samples to avoid mix-ups or contamination.
- Research the cryobank’s track record with successful pregnancies using their cryopreserved sperm. It's important to note that not all pregnancies are reported to cryobanks, and this statistic may be considerably lower than the true value.
Navigating Costs and Insurance
The services offered by cryobanks, including sperm donation, storage, and assisted reproductive procedures, come with costs. It's important to discuss these details upfront.
- Choose a cryobank that offers clear, upfront pricing for their services.
- Ask if the cryobank accepts health insurance or offers financial plans or assistance.
- Going through assisted reproduction can be emotionally taxing. A good cryobank will provide emotional and logistical support through this journey.
- Look for facilities that offer or recommend professional counseling for donors and recipients.
- Ensure your chosen cryobank has a reliable system for the shipment of sperm samples, especially if you're not located near the facility.
Choosing The Right Cryobank
Choosing the right cryobank is a pivotal decision before embarking on the journey of assisted reproduction, sperm donation, or cryopreservation. Whether you're seeking a sperm donor or are interested in becoming one, it's crucial to select a facility like Cryobank America, which demonstrates a commitment to high ethical standards, comprehensive donor screening, quality cryopreservation methods, and robust support services. Your choice will significantly impact your experience and the success of achieving your dream of starting a family or helping others.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
Freezing and Storing Sperm
Sperm freezing is a way for men to save their fertility by freezing and storing their sperm for later use. This technique has become increasingly popular as more individuals recognize the importance of maintaining their reproductive options.
It involves collecting a sperm sample from the individual and subjecting it to a series of steps that prepare it for freezing. A cryobank can store frozen sperm for many years. This storage option allows people to preserve their ability to have children. It benefits those who do not want to start a family immediately.
The history of sperm storage dates back to the 1950s when researchers began experimenting with freezing sperm. Over the years, advancements in technology and techniques have made the process more efficient and successful. Today, sperm storage is a widely accepted method for preserving fertility. Individuals who must undergo cancer treatments or individuals with medical conditions that may affect their fertility also use this method.
The Process of Freezing Sperm
The process of freezing sperm involves several steps to ensure the usability and longevity of the sperm. Once the sample is collected through masturbation, the quality and quantity of the sperm is analyzed.
After the collection and analysis, a cryoprotectant solution is added to the sample. This solution helps protect the sperm from damage during the freezing process. The mixture is divided into small vials or straws labeled and sealed for freezing.
The freezing process typically involves slowly lowering the temperature of the sperm sample to -196 degrees Celsius using liquid nitrogen. This rapid freezing technique is called vitrification.
Vitrification: Rapid Freezing Process
The process of vitrification involves several steps. First, the cells or tissues are treated with a cryoprotectant solution to dehydrate and protect them from freezing damage. Next, they are rapidly cooled to very low temperatures using liquid nitrogen or another cryogenic agent. The rapid cooling prevents the formation of ice crystals and instead forms a glass-like solid.
During vitrification, it is crucial to minimize the exposure of cells or tissues to toxic levels of cryoprotectants. A stepwise approach, where the concentration of cryoprotectants is gradually increased before vitrification, can avoid these harmful levels.
Vitrified samples stored at ultra-low temperatures remain without significant degradation. They can be rapidly thawed and rehydrated for transplantation or research purposes.
Various applications utilize vitrification. Some of these applications include the storage of embryos for in vitro fertilization (IVF), cord blood stem cells, and biological samples for research.
Benefits of Sperm Storage
Sperm storage offers several benefits to individuals who wish to preserve their fertility. One of the primary benefits is the ability to maintain reproductive options in the future. By freezing their sperm, individuals can ensure they have viable sperm available when they are ready to start a family.
Another benefit of sperm storage is the convenience and flexibility it provides. Individuals can freeze their sperm anytime, allowing them to plan for their future without the pressure of starting a family immediately. Storing sperm can benefit individuals pursuing education, career advancement, or other personal goals before beginning a family.
Additionally, sperm storage can reduce the risk of genetic abnormalities in offspring. Freezing sperm at a younger age is very beneficial. It allows individuals to preserve their sperm when it is healthier and less likely to have congenital abnormalities. Storing fertility can be vital for individuals with genetic conditions or a family history of genetic disorders.
Who Can Benefit from Sperm Storage?
Sperm storage can benefit many individuals at risk of fertility loss. It's a smart choice for those who wish to preserve their reproductive options. Some of the groups that can benefit from sperm storage include:
- Certain medical conditions, such as testicular cancer, leukemia, or autoimmune diseases, can affect sperm production or quality. By freezing their sperm before treatment, these individuals can preserve their fertility and increase their chances of having biological children.
- Men undergoing cancer treatment: Chemotherapy and radiation therapy can harm sperm production and quality. Sperm storage before cancer treatment can allow men to have biological children after completing their treatment.
- Men in high-risk occupations exposed to hazardous environments or substances may be at risk of fertility loss. By freezing their sperm, these individuals can protect their fertility and have the option to start a family.
- Men with low sperm counts or poor sperm quality may have difficulty conceiving naturally. By freezing their sperm, they can increase their chances of successful fertilization through assisted reproductive techniques.

Longevity of Frozen Sperm
The longevity of frozen sperm depends on several factors. Storage conditions and the quality of the sperm at the time of freezing are two primary factors. Generally, cryobanks can store frozen sperm for many years without significant loss of viability.
The recommended storage duration for frozen sperm varies depending on the country and the specific regulations in place. In some countries, cryobanks can store frozen sperm for up to 10 years. In other countries, cryobanks can store sperm indefinitely.
Studies have shown that using long-term frozen sperm for assisted reproductive techniques can yield successful outcomes. The success rates of using frozen sperm to achieve pregnancy are comparable to those of using fresh sperm. These rates indicate that frozen sperm can remain viable and capable of fertilization even after many years of storage.
Success Rates of Sperm Storage
The success of sperm storage depends on various factors. Sperm quality, the freezing technique used, and the laboratory's performing procedure expertise are a few factors to consider. Overall, the success rates of using frozen sperm for conception are encouraging.
Studies have shown that the survival rate of frozen sperm after thawing is typically high, ranging from 50% to 80%. Once frozen sperm is thawed, a significant portion remains viable and capable of fertilization.
The success rates of using frozen sperm for assisted reproductive techniques, such as IVF or IUI, are also promising. The chances of achieving pregnancy using frozen sperm are comparable to using fresh sperm. Frozen sperm can be just as effective in achieving conception.
Alternatives to Sperm Storage
Alternative sperm storage options are good for individuals who may not be suitable candidates for this procedure. Some of the alternatives to sperm storage include:
- Testicular Tissue Freezing may be an option for Individuals who cannot produce motile sperm. It could also benefit those at risk of losing their fertility due to medical reasons. Testicular tissue freezing involves removing a small piece of testicular tissue and freezing it for future use.
- Donor sperm is an excellent option for anyone experiencing fertility issues or same-sex couples wanting to start a family. Sperm banks have a collection of donors to choose from. The best part is they're all carefully screened and selected based on the sperm bank's standards. Donor sperm is used in home insemination, intrauterine insemination (IUI), intracervical insemination (ICI), intracytoplasmic sperm injection (ICSI), or in-vitro fertilization (IVF) procedures.
- Adoption can be an excellent option for starting a family. Individuals who cannot conceive naturally or prefer not to pursue assisted reproductive techniques can explore this. Adoption allows individuals to provide a loving home to a child in need.
Individuals must discuss their options with a fertility specialist to determine the most suitable method for preserving their fertility.
The Cost of Sperm Storage
The cost of sperm storage can vary depending on several factors. The cryobank's location, services included, and any additional procedures or tests required to determine the final cost. Sperm storage can range from $500 to $1,500, excluding extra storage or future use fees.
Cryobank America stores sperm for a one-time collection fee of $225 and a monthly storage fee of $18.99. You'll pay a one-time withdrawal fee of $399 when you are ready to use your sample.
Most insurance companies don't cover sperm storage. However, some insurance plans may cover individuals with medical conditions that affect their fertility, such as cancer. Cryobank America has partnered with LIVESTRONG Fertility, offering discounted storage services for registered patients.
Frozen Sperm For Future Fertility
Sperm storage is a valuable option for individuals who wish to preserve their fertility for future use. By freezing and storing their sperm, individuals can maintain their reproductive choices and increase their chances of having future biological children. The process of sperm storage is safe and effective, with high success rates for achieving pregnancy using frozen sperm.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States
What is A Cryobank?
A cryobank, also known as a sperm bank, is a facility that collects, processes, stores, and distributes donated sperm for use in assisted reproductive technologies. Cryobanks play a crucial role in reproductive medicine by providing individuals and couples access to donor sperm when natural conception is not possible or advisable. Cryobanks operate under strict guidelines to ensure the safety and quality of the donated sperm.
The process begins with potential donors undergoing a thorough screening to assess their physical health, medical history, and genetic background. Once accepted as donors, they provide semen samples through masturbation or other collection methods. The samples are then processed to separate the sperm from different components of semen, such as seminal fluid. The processed sperm is then frozen and stored in liquid nitrogen tanks at extremely low temperatures to maintain viability.
What Services Are Typically Offered At A Cryobank?
Semen Analysis
Semen analysis is a laboratory test that examines the characteristics of semen, which is the fluid that contains sperm. It is typically one of the first tests conducted when assessing male fertility. During a semen analysis, several parameters are examined, including sperm count, motility (movement), morphology (shape), and volume of semen. These parameters provide valuable insights into the overall health and quality of sperm.
Semen analysis results can guide fertility treatment decisions. A fertility clinic may recommend different treatment options depending on the analysis findings. For example, if the sperm count is low, assisted reproductive techniques such as intrauterine insemination (IUI) or in vitro fertilization (IVF) may be suggested. On the other hand, if sperm motility is poor, intracytoplasmic sperm injection (ICSI) may be recommended.
Advancements in technology are continuously improving the accuracy and efficiency of semen analysis. For example, computer-assisted sperm analysis (CASA) systems provide more precise measurements of sperm parameters. Ongoing research also explores new ways to assess sperm quality, such as DNA fragmentation testing. These advancements hold promise for improving male fertility assessment and treatment options.
Cryobank Donor Sperm
The process of donor sperm banking involves several steps. First, potential donors undergo a thorough screening process to see if they meet the necessary health and genetic criteria. Once approved, donors provide a semen sample through masturbation or other cryobank-approved methods.
The collected sample is then processed in a laboratory to separate the sperm from other components of semen. The sperm is then mixed with a cryoprotectant solution to protect it during freezing. The sample is divided into vials and frozen using liquid nitrogen. The vials are then stored in a cryogenic tank at extremely low temperatures to maintain the viability of the sperm.
Cryobank facilities adhere to stringent quality control measures to ensure the safety and viability of their samples. When selecting a sperm donor, cryobanks provide various services to assist prospective parents in making informed decisions.
A diverse range of individuals and couples utilizes cryobanks. Some common reasons for using donor sperm include male infertility, genetic disorders, single parenthood by choice, same-sex couples, and couples where the male partner has undergone sterilization procedures.
For individuals or couples facing male infertility, cryobanks offer a solution by providing access to donor sperm. Donor sperm allows them to pursue assisted reproductive technologies such as in vitro fertilization (IVF) or intrauterine insemination (IUI) to achieve pregnancy.
In cases where there is a risk of passing on genetic disorders, using donor sperm can help mitigate that risk. Donors are thoroughly screened for genetic conditions, reducing the chances of passing on inherited diseases to future children.
Single individuals or same-sex couples also rely on sperm banks to fulfill their desire to have children. Sperm donation allows them to start or expand their families, regardless of marital status or sexual orientation.
Click here to view Cryobank America's donor qualifications and screening requirements, or click here to begin your donor search.
Chromosome Analysis
Chromosome analysis is a method of studying genetic makeup by examining the structure and number of chromosomes. This analysis can provide valuable insights into an individual's genetic potential and help identify potential genetic disorders. Chromosome analysis uses several techniques, including karyotyping, fluorescence in situ hybridization (FISH), and comparative genomic hybridization (CGH).
Karyotyping involves staining and examining chromosomes under a microscope to determine their structure and number. This technique can help identify missing or extra chromosomes and structural abnormalities such as translocations or deletions. FISH involves using fluorescent probes to label specific genes or regions of chromosomes, allowing for the detection of specific genetic abnormalities. CGH is a technique that compares the DNA from an individual to a reference DNA sample, allowing for the detection of copy number variations or changes in the number of copies of specific genes.
Chromosome analysis has been instrumental in identifying the genetic basis of inherited traits. Researchers have identified genes contributing to traits such as eye color, height, and intelligence by studying the structure and number of chromosomes. For example, the OCA2 gene on chromosome 15 is associated with the production of melanin, which determines eye color. Variations in this gene can result in different eye colors, such as blue or brown.
Similarly, studies have identified multiple genes on different chromosomes that determine height. These genes interact with each other and environmental factors to influence an individual's height. By studying the structure and number of chromosomes, researchers can better understand the complex genetic basis of traits.

The Myriad Foresight Carrier Screening
The Myriad Foresight Carrier Screen is a cutting-edge genetic testing tool that provides comprehensive screening for over 175 genetic disorders. It utilizes advanced technology to analyze an individual's DNA and identify any mutations or variations that may indicate carrier status for a particular ailment. The Myriad Foresight Carrier Screen is highly accurate and reliable, providing individuals with valuable information about their genetic health.
One of the key advantages of the Myriad Foresight Carrier Screen is its comprehensive nature. It screens for genetic disorders, including those more prevalent in specific ethnic populations. This screening ensures that individuals receive a thorough assessment of their carrier status and can make informed decisions about their family planning options.
The Myriad Foresight Carrier Screen can detect carriers for various genetic disorders. Some specific conditions this screening can identify include cystic fibrosis, spinal muscular atrophy, sickle cell disease, and Tay-Sachs disease, among many others. These disorders vary in severity and prevalence, but all have the potential to impact an individual's health or the health of their future children.
By identifying carriers for these disorders, the Myriad Foresight Carrier Screen allows individuals to understand their risk of passing these conditions to their children. This knowledge can be invaluable in making informed decisions about family planning and taking proactive steps to safeguard the health of future generations.
Complete Bloodwork Testing
Complete bloodwork involves analyzing various components of your blood, including red blood cells, white blood cells, and platelets. Each component plays a crucial role in maintaining your overall health, and abnormalities in their levels can indicate underlying health conditions.
Red blood cells are responsible for carrying oxygen to all parts of your body. A complete blood count (CBC) measures the number of red blood cells in your blood. Abnormal levels of red blood cells can indicate anemia, which can be caused by a deficiency in iron, vitamin B12, or folic acid can cause. It can also indicate other underlying health conditions like kidney disease or bone marrow disorders.
White blood cells are essential to your immune system and help fight off infections and diseases. A CBC also measures the number of white blood cells in your blood. Elevated levels of white blood cells can indicate an infection or inflammation in your body. On the other hand, low levels of white blood cells can be a sign of a weakened immune system or certain medical conditions such as leukemia.
Platelets are responsible for clotting your blood to prevent excessive bleeding. A CBC also measures the number of platelets in your blood. Abnormal levels of platelets can indicate a bleeding disorder or a bone marrow disorder.
Cryobank Sperm Storage
Sperm storage is a critical aspect of cryobanks. Sperm can be stored in a cryobank for extended periods, allowing individuals or couples to use the sperm when they are ready to start a family.
The sperm storage process involves freezing the sperm samples in liquid nitrogen at extremely low temperatures. This freezing process helps preserve the viability of the sperm by slowing down cellular activity. Sperm can be stored in liquid nitrogen tanks for many years without significantly losing quality.
Cryobanks offer different storage options depending on individual needs and preferences. Some individuals may choose short-term storage if they plan to use the sperm within a few months or years. Others may opt for long-term storage to preserve their fertility for an extended period, such as cancer patients undergoing chemotherapy or radiation therapy.
The recommended storage duration for sperm varies depending on individual circumstances. Cryobanks can store sperm for several years without significant loss of quality. Still, it is important to consult with a fertility specialist to determine the best storage duration for your specific situation.
Known Donor Collection
Known sperm donor collection offers several benefits for families seeking to conceive through sperm donation. One of the main advantages is the potential for a stronger emotional connection and support system. When using a known sperm donor, there is the opportunity for ongoing communication and involvement between the donor, parents, and child. This involvement can create a sense of extended family and provide additional emotional support for all parties involved.
Additionally, having a known sperm donor can give families a sense of security and peace of mind. They can establish a relationship with the donor before conception, which can help build trust and ensure that the donor is a good fit for their family. Known donors are still required to undergo testing, which includes medical screening, blood testing, semen analysis, urinalysis, and more. They also have the option to receive additional screenings such as genetic testing or chromosome analysis.
Cryobank At-Home Insemination Kit
At-home insemination, also known as self-insemination, is a method used by individuals or couples trying to conceive without the assistance of a medical professional. It involves introducing sperm into the reproductive system to achieve pregnancy. Insertion is performed through various methods, such as using a sterile syringe or a cervical cap.
At-home insemination differs from other fertility treatments, such as in vitro fertilization (IVF) or intrauterine insemination (IUI) because it does not require medical intervention or fertility drugs. It is a more natural and less invasive method that individuals and couples can perform in the comfort of their own homes.
At Cryobank America, the process of at-home insemination is simple. Once you've chosen your perfect sperm donor, you'll place your vial order online. We'll schedule delivery of your vials around your schedule and fertility window. You'll receive our at-home insemination kit with everything you need to complete self-insemination. Click here for an in-depth overview of our process and steps for success.
- Protecting Your Health: Choosing A Sperm Bank Over Natural Insemination
- Hatching a Plan: Learning The Basics About Assisted Hatching in IVF
- Navigating GYN Surgery Before Artificial Insemination
- PGT Testing and Its Role in IVF Treatment
- The Ultimate Guide To Where You Can Donate Sperm In All 50 States

